Hip Bursitis | Trochanteric Bursitis
Hip Bursitis is an inflammatory painful condition at the bursa of the hip joint. There is more than a dozen bursa in the hip region. The more clinically significant ones will be discussed here.
Trochanteric bursitis is the second most frequent cause of lateral hip pain.
Hip Bursa Anatomy
Iliopsoas Bursa
Many names have been used to describe the iliopsoas bursa (IPB), including the iliopsoas, iliopectineal, iliac, iliofemoral, and subpsoas bursa.
The IPB is the largest and most constant bursa about the hip, present in 98% of normal adult individuals, usually bilaterally. The IPB is situated deep to the iliopsoas tendon and serves to cushion the tendon from the structures on the anterior aspect of the hip joint capsule. Its dimensions may be up to 7 cm in length and 4 cm in width.
See Also: Thomas Test
Anatomic boundaries of the Iliopsoas Bursa include:
- Anteriorly: the iliopsoas muscle ,
- posteriorly: the pectineal eminence and the hip joint capsule ,
- Laterally: the iliofemoral ligament ,
- Medially: the acetabular labrum.
In 15% of patients, the IPB communicates with the hip joint via a 1-mm-to-3-cm point of relative capsular thinning between the iliofemoral and pubofemoral ligaments. While this connection may occur on a congenital basis, this number rises to 30–40% in patients with hip joint pathology.
See Also: Iliacus and Psoas Major Muscles
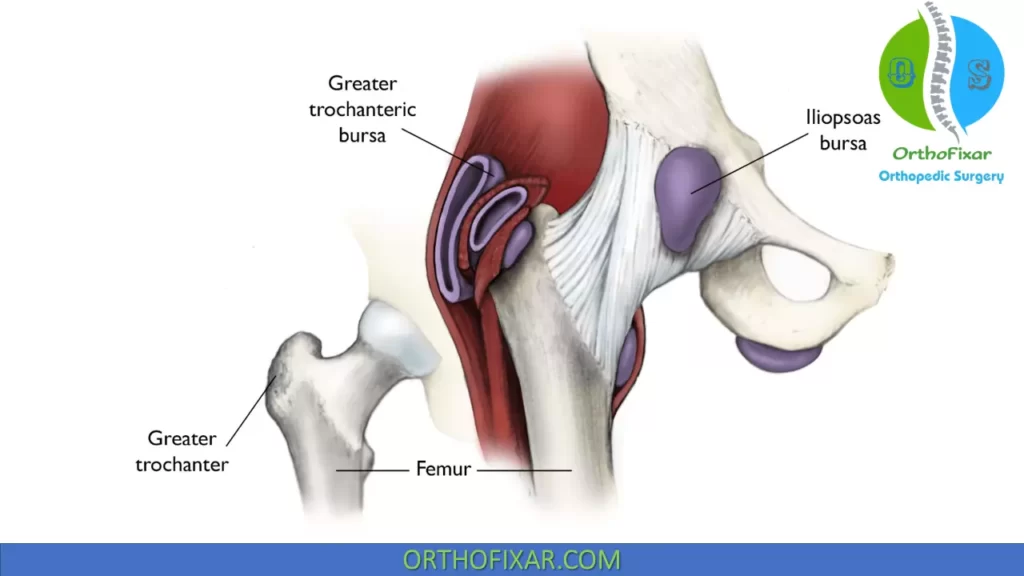
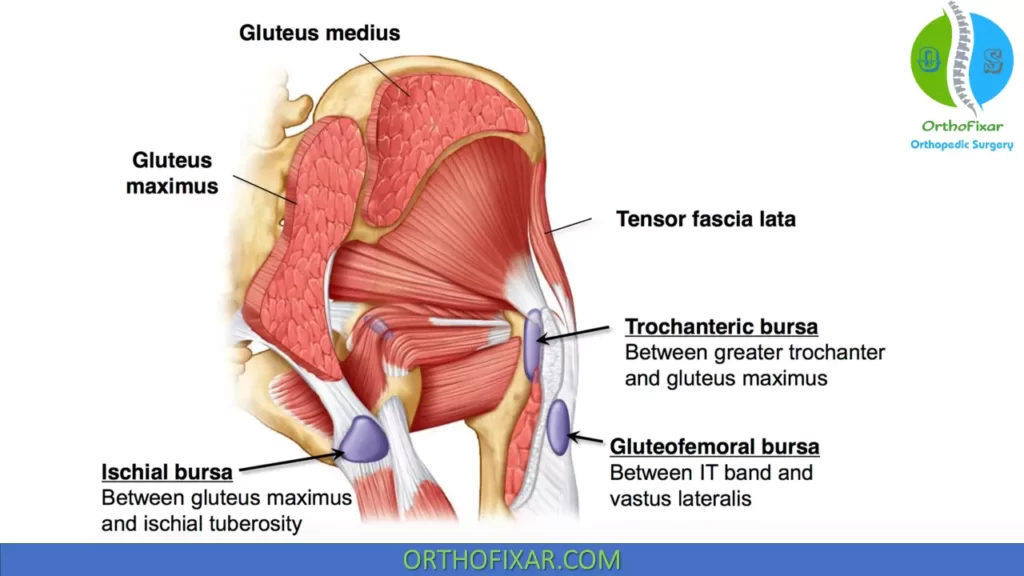
Trochanteric Bursa
Three bursae are consistently present at the greater trochanter, two major bursae and one minor bursa.
The two clinically significant trochanteric bursae are the subgluteus medius bursa, and the more superficial subgluteus maximus bursa:
- Subgluteus medius bursa: located at the superoposterior tip of the greater trochanter and functions to prevent friction between the gluteus medius muscle and the greater trochanter and also between the gluteus medius and gluteus minimus muscles.
- Subgluteus maximus bursa: located between the greater trochanter and the fibers of the gluteus maximus and tensor fascia lata muscles as they blend into the ITB.
Ischiogluteal Bursa
The Ischiogluteal bursa is located between the ischium and the gluteus maximus muscle. It can be painfully squeezed between the ischial tuberosity and the hard surface of a chair during sitting, producing an ischial bursitis. This condition is often referred to as weaver’s bottom.
See Also: Hip Muscles Anatomy
Types of Hip Bursitis
Trochanteric Bursitis / Subtrochanteric Bursitis
Trochanteric bursitis is the shared name given to inflammation of any one of the three trochanteric bursae. It has been suggested that trochanteric bursitis should be considered as a clinical diagnosis rather than an anatomical diagnosis, because it cannot be distinguished from gluteal tendinitis by signs and symptoms alone.
Greater Trochanteric bursitis is the second most frequent cause of lateral hip pain, with a peak incidence occurring between 40 and 60 years of age, and is more common in arthritic conditions and fibromyalgia and leg length discrepancy. It is also more common in females than males (2–4:1 ratio).
The greater trochanteric bursa can become inflamed through either friction or direct trauma, such as a fall on the side of the hip.
The history may reveal complaints of aching lateral thigh, groin, and gluteal pain, especially when lying on the involved side. Although the pain is typically local to the hip region, it can radiate distally to the knee and the lower leg.
Objectively, the clinical findings include:
- the reproduction of pain with palpation or with stretching of the ITB across the trochanter with hip adduction or the extremes of internal or external hip rotation;
- the resisted abduction, extension, or external rotation of the hip are also painful;
- there is often associated tightness of the hip adductors, which cause the patient’s feet to cross the midline, resulting in increased stress on the trochanteric bursa.
Differential diagnosis should include:
- tendopathy of the gluteus medius or maximus muscles, with or without calcification;
- inguinal and femoral hernia;
- an irritation of the L4–5 nerve root;
- meralgia paresthetica;
- a snapping hip;
- lower spinal neoplasm;
- pelvic tumor;
- hip infection;
- avascular necrosis;
- stress fracture of the femur;
- bone or soft tissue tumor.
There is very little research on physical therapy treatment for trochanteric bursitis.
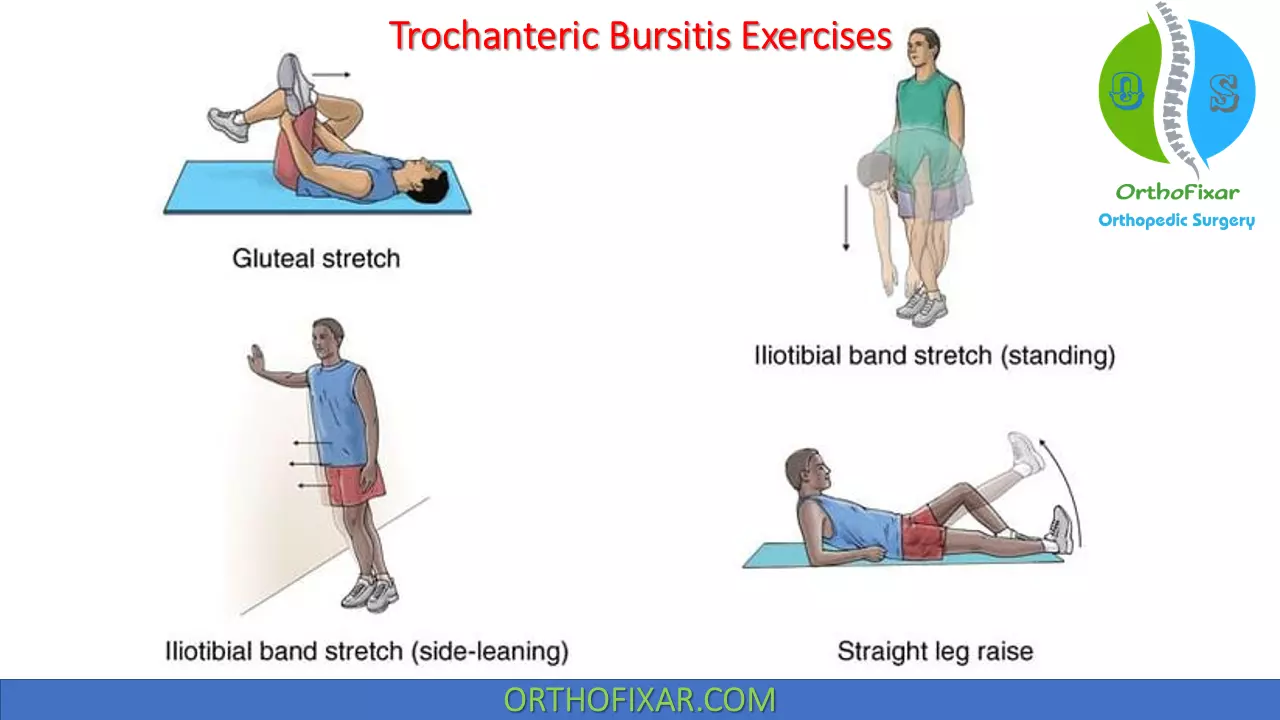
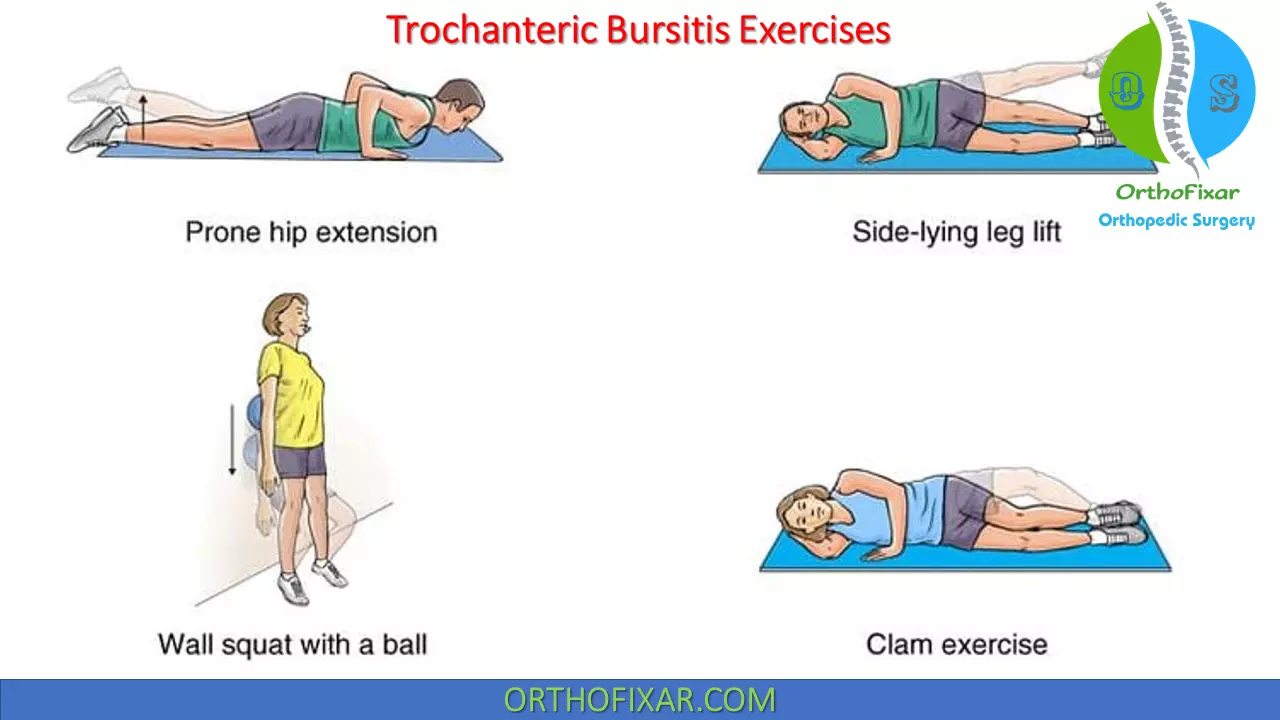
The Trochanteric Bursitis treatment typically consists of:
- Removal of the causative factors by stretching the lateral thigh tissues, especially the TFL and ITB, and emphasizing flexibility of the external rotators, quadriceps, and hip flexors.
- Strengthening of the hip abductors and correction of any muscle imbalances between the adductors and abductors is also important.
- Heat and ultrasound.
- Orthotics may be prescribed if there is a biomechanical fault in the kinetic chain.
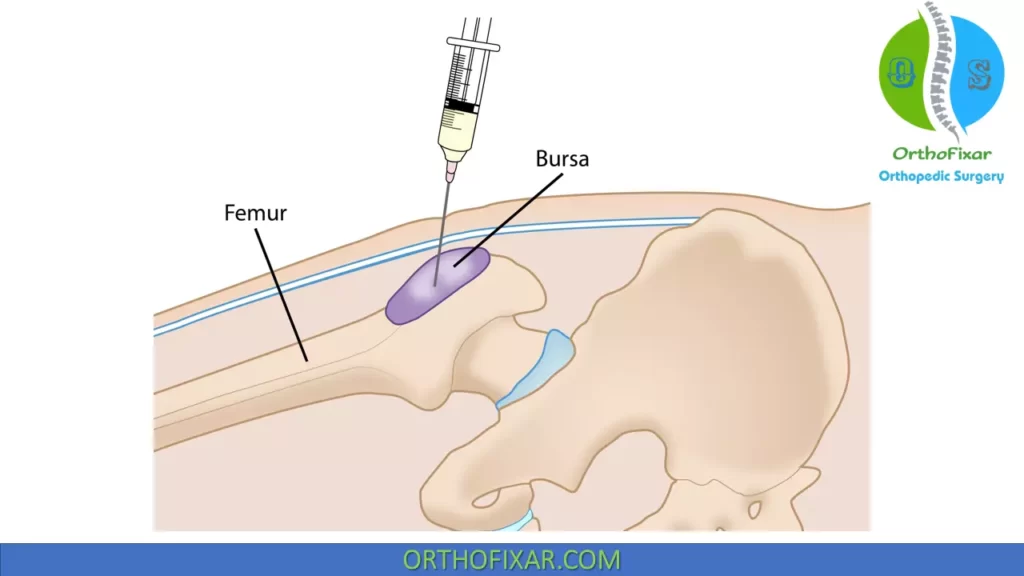
- A steroid injection at the area of tenderness over the greater trochanter may be useful in particularly intense or recalcitrant cases.
Iliopsoas Bursitis / Iliopectineal Bursitis
Iliopsoas bursitis seems to be under-recognized by the medical community despite reports that continue to be published. This may be because the entity often exists for years without being identified.
The usual complaint is one of anterior hip or groin pain, which is aggravated by lumbar or hip hyperextension or power walking. In the older populations, Iliopsoas bursitis can mimic such conditions as hip joint pathology, an L2–3 nerve root pathology, and meralgia paresthetica.
Clinical findings are few, and they include:
- pain with passive hip flexion and adduction at the end range;
- pain with passive hip extension and external rotation, which is increased if the hip flexors are resisted in this position;
- palpable tenderness of the involved bursa.
Iliopsoas Bursitis treatment consists of stretching and strengthening program of the hip rotators and hip flexors.
The recommended protocol for Iliopsoas Bursitis exercises include:
- seated hip internal and external elastic resistance exercises;
- side-lying abduction/external rotation elastic resistance exercises;
- mini-squats, weight-bearing on the affected leg;
- stretching of the hip flexor, quadriceps, and lateral hip/ piriformis, and hamstring muscles.
Ischial Bursitis
An ischial bursitis, also referred to as Weaver’s bottom, involves two different bursae:
- one between the ischial tuberosity and the inferior part of the gluteus maximus belly,
- the other between the tendons of the biceps femoris and semimembranosus.
Inflammation of these bursae usually results from chronic compression or direct trauma. Ischial bursitis tends to affect thinner people more than obese individuals and women more than men. It is also common in cyclists.
Clinically, the patient typically reports pain with sitting in a firm chair, almost as soon as the buttocks touch the chair.
Differential diagnosis should include:
- lumbar nerve root impingement,
- hamstring syndrome,
- piriformis syndrome,
- hamstring insertion tendopathy.
These can be differentiated between using the history, palpation, and resistive testing, as patients with ischial bursitis generally will not complain of pain in the posterior thigh or demonstrate hamstring flexibility and strength inadequacies.
See Also: Hamstring Flexibility Test
Ischial Bursitis treatment is based on the cause, and typically involves:
- Relative rest,
- the use of a padded seat cushion,
- soft tissue massage,
- correction of hamstring strength and flexibility deficits,
- anti-inflammatory measures such as ice massage,
- ultrasound.
- A steroid injection

Gluteal Bursitis
Inflammation of the gluteal bursa, which is located above and behind the greater trochanter, and underneath the gluteus maximus and medius, is one of the most frequent causes of pseudoradicular pain in the lower extremity.
The patient, who is usually in their fourth or fifth decade, typically complains of pain in the gluteal or trochanteric area, which may spread to the outer or posterior thigh, and down to the calf muscles and the malleolus. Unlike the pain caused by a lumbar disk lesion, the symptoms are not related to sitting, but only to walking and going up stairs.
A typical pattern is pain on passive internal rotation and abduction, and resisted external rotation or abduction.
Gluteal Bursitis treatment is based on the cause, and usually involves:
- The use of a padded seat cushion,
- Anti-inflammatory measures such as ice massage,
- Ultrasound.
References
- Shbeeb MI, Matteson EL. Trochanteric bursitis (greater trochanter pain syndrome). Mayo Clin Proc. 1996 Jun;71(6):565-9. doi: 10.4065/71.6.565. PMID: 8642885.
- Melamed A, Bauer C, Johnson H: Iliopsoas bursal extension of arthritic disease of the hip. Radiology 89:54–58, 1967.
- Armstrong P, Saxton H: Ilio-psoas bursa. Br J Radiol 45:493–495, 1972.
- Chandler SB: The iliopsoas bursa in man. Anat Rec 58:235–240, 1934
- Sartoris DJ, Danzig L, Gilula L, et al: Synovial cysts of the hip joint and iliopsoas bursitis: a spectrum of imaging abnormalities. Skeletal Radiol 14:85–94, 1985.
- Yamamoto T, Marui T, Akisue T, et al: Dumbbell-shaped iliopsoas bursitis penetrating the pelvic wall: a rare complication of hip arthrodesis. A case report. J Bone Joint Surg Am 85-A:343–345, 2003.
- Fagerson TL: Hip pathologies: diagnosis and intervention. In: Magee DJ, Zachazewski JE, Quillen WS, eds. Pathology and Intervention in Musculoskeletal Rehabilitation. St. Louis, MO: Saunders, 2009:497–527.
- Roberts WN, Williams RB: Hip pain. Primary Care 15:783–793, 1988.
- Hammer WI: The use of transverse friction massage in the management of chronic bursitis of the hip or shoulder. J Man Physiol Ther 16:107–111, 1993.
- Buckingham RB: Bursitis and tendinitis. Compr Ther 7:52–57, 1981.
- Cibulka MT, Delitto A: A comparison of two different methods to treat hip pain in runners. J Orthop Sports Phys Ther 17:172–176, 1993.
- Johnston CAM, Kindsay DM, Wiley JP: Treatment of iliopsoas syndrome with a hip rotation strengthening program: a retrospective case series. J Orthop Sports Phys Ther 29:218–224, 1999.
- Gordon EJ: Trochanteric bursitis and tendinitis. Clin Orthop 20:193– 202, 1961.
- Lifetime product updates
- Install on one device
- Lifetime product support
- Lifetime product updates
- Install on one device
- Lifetime product support
- Lifetime product updates
- Install on one device
- Lifetime product support
- Lifetime product updates
- Install on one device
- Lifetime product support