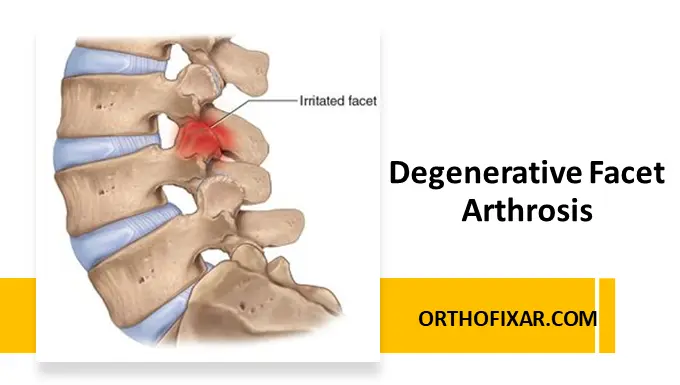
What Is Degenerative Facet Arthrosis?
Degenerative facet arthrosis, also known as facet joint osteoarthritis, is a chronic degenerative condition affecting the facet joints of the spine. These joints are located at the back of the vertebrae and play a crucial role in guiding spinal movement and providing stability.
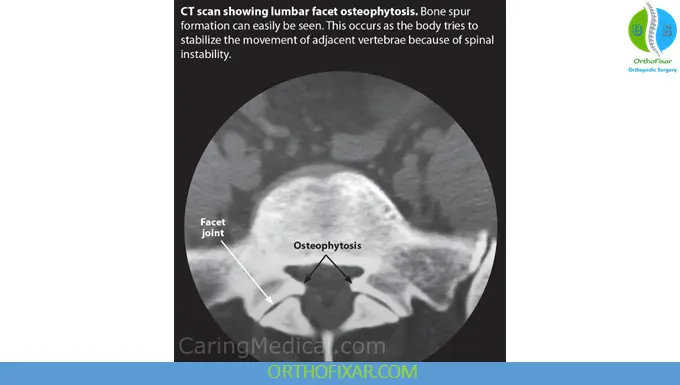
Over time, age-related wear and tear can lead to cartilage degeneration, joint space narrowing, and bony overgrowth (osteophyte formation). This process may result in pain, stiffness, and reduced spinal mobility.
Facet arthrosis commonly affects the cervical (neck) and lumbar (lower back) regions and is a frequent cause of chronic axial spine pain.
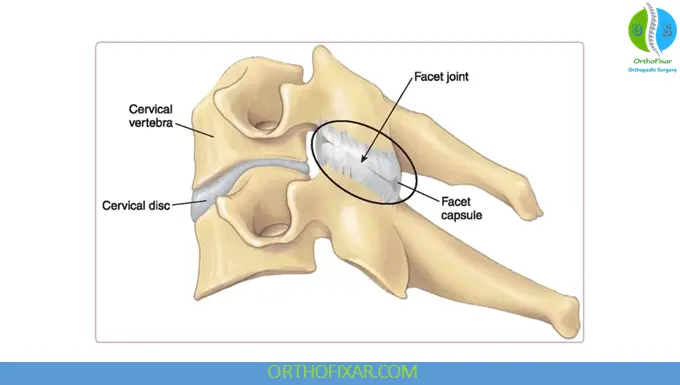
Anatomy of the Facet Joints
Facet joints (zygapophyseal joints) are synovial joints formed between the superior and inferior articular processes of adjacent vertebrae. Each spinal segment contains a pair of facet joints, allowing controlled movement while limiting excessive rotation and shear forces.
Healthy facet joints are covered with smooth cartilage and surrounded by a joint capsule. Degeneration of these structures leads to arthrosis and inflammation.
Causes and Risk Factors
Degenerative facet arthrosis usually develops gradually and may be influenced by several factors:
- Aging – natural cartilage wear with time
- Repetitive spinal loading – heavy lifting or poor posture
- Previous spinal injury or trauma
- Degenerative disc disease – increased load on facet joints
- Obesity – added mechanical stress on the spine
- Genetic predisposition
- Sedentary lifestyle or poor core stability
See Also: Facet Joint Dysfunction
Signs and Symptoms
Symptoms vary depending on the spinal level involved and the severity of degeneration.
Common Symptoms Include:
- Localized neck or lower back pain
- Pain worsened by extension, rotation, or prolonged standing
- Morning stiffness that improves with movement
- Reduced range of motion
- Tenderness over the affected spinal segment
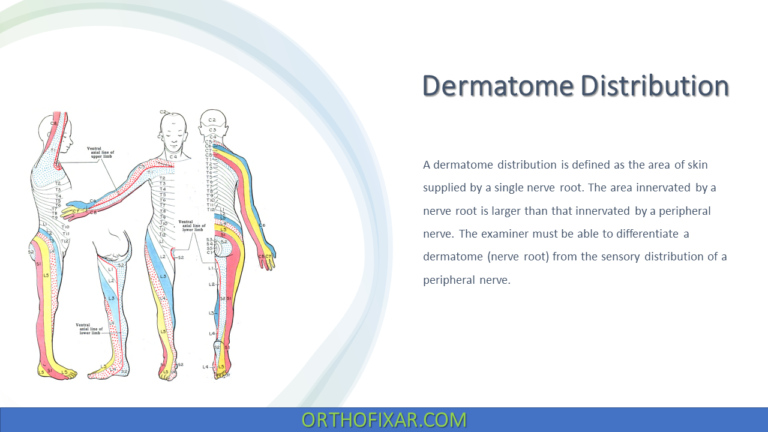
Cervical Facet Arthrosis:
- Neck pain radiating to shoulders or upper back
- Headaches (cervicogenic in origin)
- Pain aggravated by turning the head
Lumbar Facet Arthrosis:
- Lower back pain without true radicular symptoms
- Pain increased with standing or walking
- Relief when sitting or bending forward
Unlike disc herniation, facet arthrosis typically does not cause significant neurological deficits unless associated with spinal stenosis.
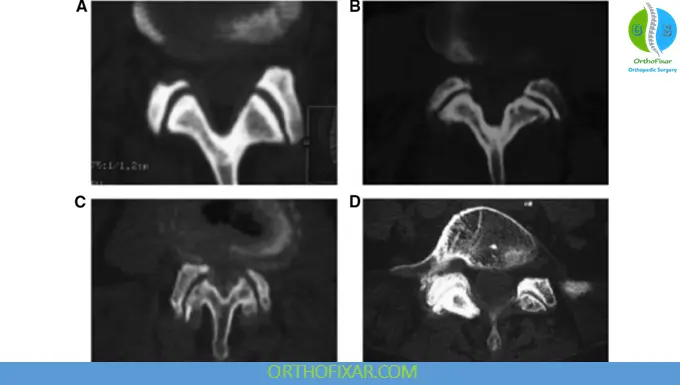
Facet Arthropathy Grading
The Pathria et al. classification system is a widely used 4-grade scale for evaluating facet joint (FJ) arthropathy, or osteoarthritis (OA), primarily using computed tomography (CT) and, in some contexts, plain radiographs:
- Grade I (Normal/Mild): Normal facet joint space (typically 2-4 mm), with no, or minimal, osteophytes and/or mild articular process hypertrophy. Some sources define this as mild, noting joint space narrowing.
- Grade II (Moderate): Mild to moderate joint space narrowing ((<2) mm) with subchondral sclerosis, and/or small osteophytes, and/or mild articular process hypertrophy.
- Grade III (Severe): Further joint space narrowing ((<1) mm or “bone to bone”), with subchondral sclerosis, and/or moderate osteophytes.
- Grade IV (Very Severe): Severe osteoarthritis with complete absence of joint space (arthrodesis or “bone on bone”) and/or large osteophytes.
Diagnosis
Diagnosis is based on a combination of clinical examination and imaging studies.
Clinical Assessment:
- Pain pattern and aggravating movements
- Palpation for localized tenderness
- Assessment of spinal range of motion
- Neurological examination (usually normal)
Imaging:
- X-rays: show joint space narrowing, sclerosis, and osteophytes
- CT scan: detailed visualization of bony changes
- MRI: useful to assess soft tissues, inflammation, and rule out other causes
In some cases, diagnostic facet joint injections are used to confirm the pain source.
Management and Treatment Options
Treatment of degenerative facet arthrosis is usually conservative, especially in early and moderate cases.
Conservative Management:
- Activity modification and posture correction
- Physiotherapy focusing on mobility, stabilization, and core strengthening
- Heat or cold therapy
- Non-steroidal anti-inflammatory drugs (NSAIDs)
- Muscle relaxants (if indicated)
Interventional Treatments:
- Facet joint steroid injections
- Medial branch nerve blocks
- Radiofrequency ablation (for chronic, refractory pain)
Surgical Treatment:
Surgery is rarely indicated and is considered only when facet arthrosis is associated with significant spinal instability or stenosis not responding to conservative care.
Role of Rehabilitation
Rehabilitation plays a key role in long-term symptom control. A structured program may include:
- Spinal mobility exercises
- Postural re-education
- Core and paraspinal muscle strengthening
- Ergonomic advice for daily activities
- Weight management strategies
Regular exercise helps reduce joint stress and improves spinal function.
Prognosis
Degenerative facet arthrosis is a chronic but manageable condition. With appropriate treatment and lifestyle modification, most patients experience significant symptom relief and improved quality of life.
Early diagnosis and adherence to conservative care are essential to prevent progression and chronic pain.
Key Takeaway
Degenerative facet arthrosis is a common cause of neck and back pain, especially in older adults. Understanding the condition, recognizing symptoms early, and following a structured management plan can significantly reduce pain and improve function.
References & More
- Anterior column reconstruction of the lumbar spine in the lateral decubitus position: anatomical and patient-related considerations for ALIF, anterior-to-psoas, and transpsoas LLIF approaches – Scientific Figure on ResearchGate. Available from: Researchgate
- Curtis L, Dua A, Shah N, et al. Facet Joint Disease. [Updated 2025 Mar 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: Pubmed
- Mann SJ, Viswanath O, Singh P. Lumbar Facet Arthropathy. [Updated 2023 Jul 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: Pubmed
- Su DCJ, Chang KV. Facet Arthritis. [Updated 2023 Jul 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: Pubmed