Egawa Sign is a specific clinical examination technique used to assess the function of the interosseous muscles and detect ulnar nerve palsy. This test provides valuable diagnostic information about the integrity of the deep branch of the ulnar nerve, which innervates the interosseous muscles of the hand.
The interosseous muscles consist of four dorsal and three palmar interossei, all innervated by the deep branch of the ulnar nerve. The dorsal interossei are responsible for finger abduction, while the palmar interossei control finger adduction. These muscles also provide fine motor control and coordination of finger movements while stabilizing the metacarpophalangeal joints during grip activities.
See Also: Palmar Interossei of Hand
See Also: Dorsal Interossei of Hand
How to Perform the Egawa Sign Test?
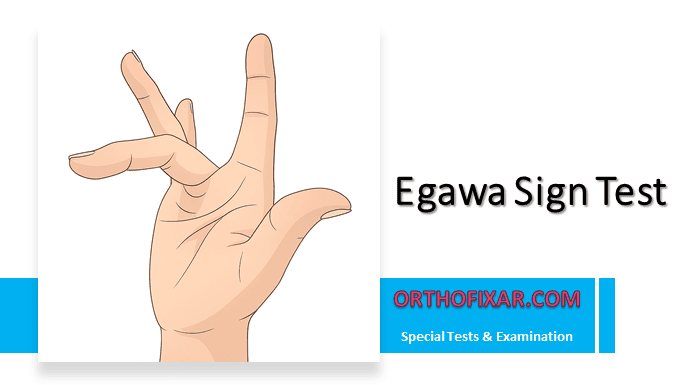
The examination begins with the patient sitting comfortably, hand resting on a flat surface with the palm down. The examiner instructs the patient to flex the middle finger at the metacarpophalangeal joint while keeping the interphalangeal joints extended. With the MCP joint maintained in flexion, the patient is then asked to move the middle finger toward the radial side, then toward the ulnar side, creating an alternating abduction movement. The key is the patient’s ability to smoothly alternate between radial and ulnar deviation while maintaining stable MCP flexion.

What is the result of the Egawa Sign Test?
A negative Egawa Sign demonstrates intact interosseous muscle function, with the patient able to maintain stable MCP flexion while smoothly performing alternating abduction movements without difficulty or weakness. Conversely, a positive sign indicates compromised interosseous function and suggests ulnar nerve palsy.
Positive Egawa Sign Test manifests as inability to perform the alternating movements, weakness or absence of deviation, difficulty maintaining the required joint position, or tremor and instability during attempted movements.
Clinical Significance
Egawa Sign holds particular value in clinical practice because the interosseous muscles are among the first to be affected in ulnar nerve compression. This makes the test especially useful for early diagnosis before more obvious signs of ulnar neuropathy develop. The positive sign helps localize the lesion specifically to the deep branch of the ulnar nerve, distinguishing it from more proximal ulnar nerve injuries or other neurological conditions. Additionally, the test can be performed serially to monitor disease progression or track recovery following treatment interventions.
Differential Diagnosis
When Egawa Sign is positive, clinicians should consider ulnar nerve palsy as the most common cause, though cubital tunnel syndrome and Guyon’s canal syndrome are also possibilities. Cervical radiculopathy affecting the C8-T1 nerve roots can produce similar findings, as can brachial plexopathy. While anterior interosseous nerve syndrome might be considered, it typically affects different muscle groups and would not produce a positive Egawa Sign.
See Also: Ulnar Nerve Anatomy & Function
Associated Clinical Findings
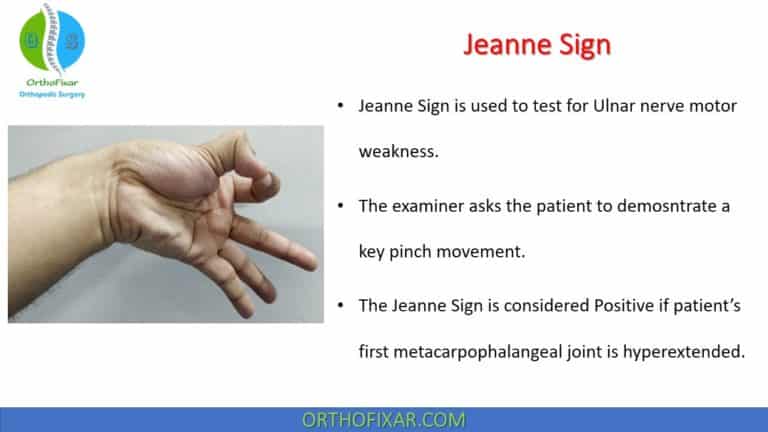
Patients demonstrating a positive Egawa Sign frequently exhibit other signs of ulnar nerve dysfunction. Froment’s sign may be present, where the patient compensates for weak thumb adduction by flexing the thumb during lateral pinch.
Wartenberg’s sign, characterized by persistent abduction of the little finger, is another common finding. More advanced cases may show claw hand deformity with hyperextension at the metacarpophalangeal joints and flexion at the interphalangeal joints. Patients often report weakness in grip strength and difficulty with fine motor tasks, along with sensory loss in the ulnar nerve distribution.
Clinical Considerations
The test achieves optimal sensitivity when performed slowly and deliberately, allowing the examiner to appreciate subtle weakness or coordination deficits. Comparing both hands often reveals asymmetries that might be missed when examining a single hand. The degree of weakness or complete inability to perform the movements should be carefully documented. Even if some movement remains possible, significant asymmetry between hands should be considered a positive test result. In cases of early ulnar neuropathy, Egawa Sign may demonstrate greater sensitivity than standard grip strength measurements.
Limitations and Interpretive Challenges
The test requires patient cooperation and clear understanding of the instructions, which may limit its utility in certain populations. Patients with significant hand deformities may find the test difficult to perform, potentially affecting interpretation. Pre-existing arthritis or other joint conditions can complicate results, as joint stiffness or pain may interfere with movement rather than indicating nerve dysfunction. Additionally, anatomical variations between individuals may influence test results, requiring clinical correlation with other examination findings and patient history.
References & More
- Beutel BG, Worley C, Hosseinzadeh S. Intrinsic Hand Deformity. [Updated 2024 Nov 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: PubMed
- Jennings JD, Jennings JF. Isolated Compression of the Ulnar Nerve Motor Branch: A Case Series With 3 Unique Etiologies. Ann Plast Surg. 2018 May;80(5):529-532. doi: 10.1097/SAP.0000000000001406. PMID: 29489540. PubMed
- Goldman SB, Brininger TL, Schrader JS, Koceja DM: A review of clinical tests and signs for the assessment of ulnar neuropathy, J Hand Ther 22(3):209–220, 2009.
- Orthopedic Physical Assessment by David J. Magee, 7th Edition.