Musculocutaneous nerve injury represents an uncommon but clinically significant peripheral nerve disorder that can substantially impact upper extremity function. While less frequently encountered than other brachial plexus injuries, understanding the anatomy, pathophysiology, and clinical manifestations of musculocutaneous nerve damage is essential for accurate diagnosis and effective patient management.
Anatomical Foundation and Clinical Significance
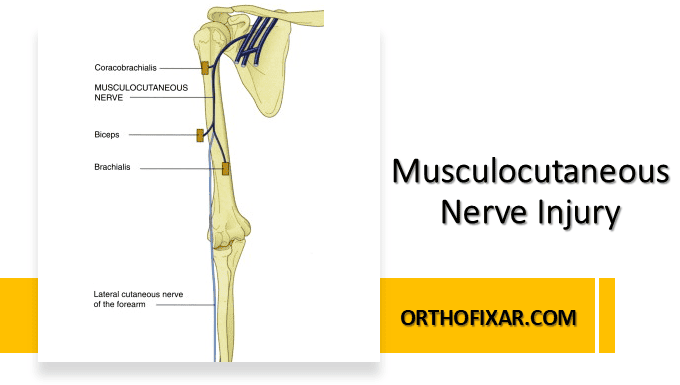
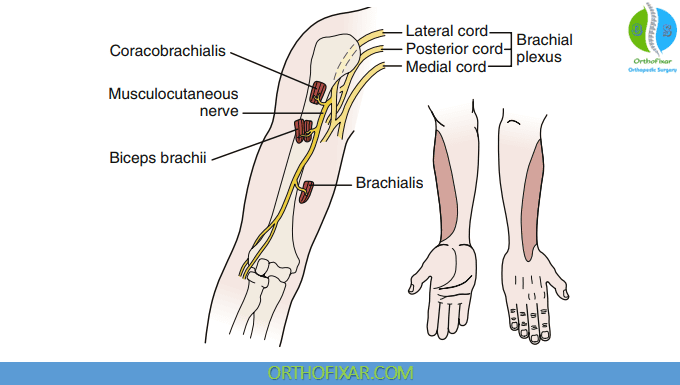
The musculocutaneous nerve originates from the lateral cord of the brachial plexus, specifically from nerve roots C5, C6, and C7. This nerve provides motor innervation to three critical muscles of the anterior arm compartment: the coracobrachialis, biceps brachii, and brachialis. Additionally, the nerve gives rise to the lateral antebrachial cutaneous nerve, which provides sensory innervation to the anterolateral aspect of the forearm.
The clinical importance of this nerve becomes apparent when considering its role in fundamental upper extremity movements. The musculocutaneous nerve is responsible for elbow flexion through the biceps brachii and brachialis muscles, shoulder forward flexion via the biceps brachii and coracobrachialis, and contributes significantly to forearm supination through the biceps brachii muscle.
See Also: Brachial Plexus Anatomy Overview
Mechanisms of Musculocutaneous Nerve Injury
Musculocutaneous nerve injury typically occurs through several distinct mechanisms. Traumatic injuries represent the most common cause, with humeral dislocations and fractures being particularly implicated. The nerve’s anatomical course makes it vulnerable during shoulder dislocations, especially anterior dislocations where the humeral head may compress or stretch the nerve against surrounding structures.
Brachial plexus injuries frequently involve the musculocutaneous nerve due to its origin from the lateral cord. High-energy trauma such as motorcycle accidents, falls from height, or birth trauma can result in complex nerve injuries affecting multiple components of the brachial plexus, including the musculocutaneous nerve.
Vascular complications can also lead to musculocutaneous nerve dysfunction. Injuries to the adjacent axillary artery may result in ischemic damage to the nerve, either through direct compression from hematoma formation or through compromised blood supply to the neural tissues.
Clinical Presentation and Functional Deficits
The clinical presentation of musculocutaneous nerve injury is characterized by specific motor and sensory deficits that reflect the nerve’s anatomical distribution. Motor dysfunction primarily manifests as weakness in elbow flexion, which becomes particularly apparent when patients attempt to flex the elbow against resistance. The biceps brachii and brachialis muscles, both innervated by the musculocutaneous nerve, are the primary elbow flexors, and their weakness significantly impairs this fundamental movement.
Shoulder forward flexion weakness is another prominent feature, as the coracobrachialis and biceps brachii muscles contribute to this motion. Patients may demonstrate difficulty lifting objects or reaching forward, particularly when these movements require significant force generation.
Supination strength is notably diminished due to biceps brachii weakness. While the supinator muscle, innervated by the posterior interosseous nerve, can still perform supination, the loss of biceps contribution results in measurable weakness during clinical testing.
The sensory component of musculocutaneous nerve injury involves the lateral antebrachial cutaneous nerve, which provides sensation to the anterolateral aspect of the forearm. Patients typically report numbness, tingling, or altered sensation in this distribution, which can be confirmed through sensory testing during physical examination.
Musculocutaneous Nerve Tunnel Syndrome
A distinct clinical entity that merits special attention is musculocutaneous nerve tunnel syndrome, specifically involving compression of the lateral antebrachial cutaneous nerve. This condition occurs when the sensory branch becomes compressed as it passes beneath the distal biceps tendon, creating a localized entrapment neuropathy.
The pathophysiology of this syndrome often involves repetitive activities that place stress on the nerve at this anatomical location. Forced elbow hyperextension can stretch the nerve against the biceps tendon, while repeated pronation movements, such as those involved in excessive screwdriving or backhand tennis strokes, can create chronic compression and irritation.
Clinically, musculocutaneous nerve tunnel syndrome presents primarily with sensory symptoms in the lateral forearm distribution. Patients may experience burning pain, numbness, or paresthesias that can be exacerbated by the precipitating activities. This condition is frequently misdiagnosed as lateral epicondylitis (tennis elbow) due to the similarity in symptom location and the common association with tennis and other racquet sports.
Diagnostic Approach and Clinical Assessment
Accurate diagnosis of musculocutaneous nerve injury requires a comprehensive clinical evaluation that includes detailed history taking, physical examination, and appropriate diagnostic testing. The history should focus on identifying potential traumatic events, repetitive activities, or associated injuries that might explain the nerve dysfunction.
Physical examination should systematically assess motor function through specific muscle testing. Elbow flexion strength testing with the forearm in supination preferentially activates the biceps brachii, while testing with the forearm in pronation better isolates the brachialis muscle. Shoulder forward flexion can be assessed through standard range of motion testing with resistance applied.
Sensory examination should include light touch, pinprick, and two-point discrimination testing in the lateral antebrachial cutaneous nerve distribution. Provocative maneuvers, such as elbow hyperextension or forced pronation, may reproduce symptoms in cases of nerve tunnel syndrome.
Electrodiagnostic studies, including nerve conduction studies and electromyography, provide objective confirmation of nerve dysfunction and can help localize the site of injury. These studies are particularly valuable in distinguishing musculocutaneous nerve injuries from other causes of elbow flexion weakness or forearm sensory symptoms.
Advanced imaging, including magnetic resonance imaging or ultrasound, may be helpful in identifying structural abnormalities, space-occupying lesions, or anatomical variants that contribute to nerve compression.
Treatment Strategies and Management Principles
Management of musculocutaneous nerve injury depends on the underlying etiology, severity of dysfunction, and timing of presentation. Conservative management is often the initial approach, particularly for cases involving mild compression or incomplete nerve injuries.
Activity modification plays a crucial role in conservative treatment, especially for cases of nerve tunnel syndrome. Patients should avoid or modify activities that exacerbate symptoms, such as repetitive pronation or forced elbow hyperextension. Ergonomic adjustments in occupational or recreational activities may be necessary to prevent symptom recurrence.
Physical therapy intervention focuses on maintaining range of motion, strengthening unaffected muscles, and promoting functional adaptation. Therapists may employ nerve mobilization techniques and progressive strengthening exercises as appropriate for the individual patient’s condition and recovery stage.
Anti-inflammatory medications may provide symptomatic relief, particularly in cases where inflammation contributes to nerve compression. Neuropathic pain medications may be considered for patients experiencing significant sensory symptoms or neuropathic pain.
Surgical intervention may be necessary in cases of complete nerve transection, severe compression with progressive weakness, or failure to respond to conservative management. Surgical options include nerve decompression, nerve repair, or nerve grafting, depending on the specific pathology encountered.
Prognosis and Recovery Expectations
The prognosis for musculocutaneous nerve injury varies significantly based on the mechanism of injury, completeness of nerve dysfunction, and timeliness of appropriate treatment. Incomplete injuries or cases involving primarily demyelination tend to have better recovery potential compared to complete axonal injuries.
Recovery from peripheral nerve injuries follows predictable patterns based on the biology of nerve regeneration. Sensory recovery typically precedes motor recovery, and proximal muscles generally recover before distal muscles. The rate of nerve regeneration is approximately one millimeter per day, which helps establish realistic expectations for functional recovery timelines.
Factors that influence prognosis include patient age, with younger patients generally demonstrating better recovery potential, the presence of associated injuries, and the adequacy of rehabilitation efforts. Early recognition and appropriate management significantly improve outcomes and reduce the likelihood of permanent functional deficits.
Conclusion
Musculocutaneous nerve injury, while uncommon, represents an important clinical entity that requires prompt recognition and appropriate management. Understanding the anatomical basis, clinical presentation, and treatment options enables healthcare providers to optimize patient outcomes and minimize long-term functional impairment. The distinction between traumatic nerve injuries and entrapment syndromes such as musculocutaneous nerve tunnel syndrome is crucial for implementing appropriate treatment strategies and setting realistic recovery expectations.
Resources
- Orthopedic Physical Assessment by David J. Magee, 7th Edition.
- Neal S, Fields KB. Peripheral nerve entrapment and injury in the upper extremity. Am Fam Physician. 2010 Jan 15;81(2):147-55. PMID: 20082510. Pubmed
- Kissel JA, Leonardelli C. Isolated musculocutaneous neuropathy: a case report. J Can Chiropr Assoc. 2019 Dec;63(3):162-170. PMID: 31988537; PMCID: PMC6973755. Pubmed
- Desai SS, Arbor TC, Varacallo MA. Anatomy, Shoulder and Upper Limb, Musculocutaneous Nerve. [Updated 2023 Sep 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: Pubmed