Diagnostic imaging is used in conjunction with a physical examination to determine a diagnosis. It should never be used in isolation, but any findings should be related to clinical signs to rule out false-positive indications or age-related changes.
The shoulder joint’s complex anatomy and wide range of motion require multiple shoulder X-ray views to fully evaluate potential pathology.
Shoulder X-ray Views
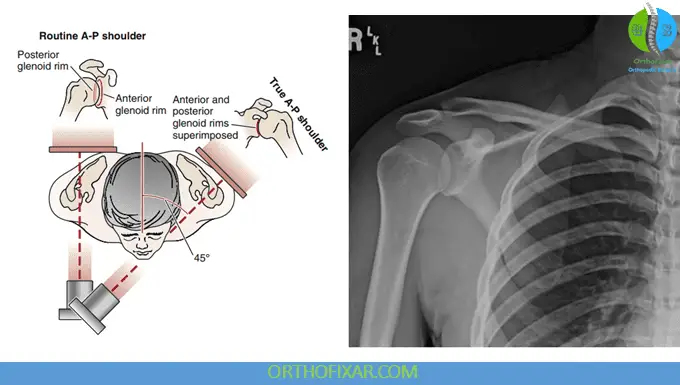
Anteroposterior (AP) View
This projection can be obtained as either a true AP view or a tilt view.
Clinical Applications and Assessment Points
The shoulder AP view allows comprehensive evaluation of several critical anatomical relationships and pathological conditions that include:
1. Glenohumeral Joint Assessment: One of the most important diagnostic signs to recognize is the “empty glenoid” sign, which may indicate posterior shoulder dislocation. In normal anatomy, the radiograph demonstrates overlapping shadows of the humerus and glenoid. When a posterior dislocation occurs, this shadow becomes reduced or completely absent, creating the characteristic empty appearance of the glenoid fossa.
See Also: Glenohumeral Joint Anatomy
2. Acromioclavicular Joint Evaluation: The AP view provides excellent visualization for assessing acromioclavicular joint width, identifying spurring of the undersurface, evaluating lateral tilt of the acromion, and measuring the critical distance between the humeral head and anterior acromion.
3. Epiphyseal Plate Analysis: Particularly important in pediatric and adolescent patients, the examiner should determine the presence and normalcy of the humeral head epiphyseal plate, which can provide valuable information about growth patterns and potential growth disturbances.
4. Calcific Tendinopathy Detection: The shoulder AP view is excellent for identifying calcifications within the rotator cuff tendons, particularly the supraspinatus and infraspinatus muscles. These calcifications can be indicators of chronic tendinopathy or calcific tendinitis.
5. Acromial Morphology Assessment The configuration of the acromion’s undersurface is an important cause of impingement syndrome of the shoulder. The AP view allows evaluation of acromial shape and the presence of subacromial spurs, which can contribute to rotator cuff pathology.
See Also: Rotator Cuff of the Shoulder
Key Diagnostic Findings
Hill-Sachs Lesion Identification: When the humerus is positioned in medial rotation during AP imaging, a defect may become visible on the lateral aspect of the humeral head. This defect, known as a Hill-Sachs lesion, represents a compression fracture of the postero-superolateral humeral head resulting from recurrent anterior dislocations. These lesions are classified as either engaged or nonengaged, with engaged lesions articulating with the glenoid during arm abduction and lateral rotation, potentially affecting joint stability.
Reverse Hill-Sachs Lesions: In cases of posterior dislocation, an anteromedial humeral head impression fracture may occur, known as a reverse Hill-Sachs lesion (RHSL), Malgaigne lesion, or McLaughlin lesion. These lesions occur in 30% to 90% of posterior dislocations and can be visualized on plain radiographs, CT scans, or MRI.
Acromiohumeral Interval Measurement: The space between the acromion and humerus, known as the acromiohumeral interval, should measure between 7-14 mm under normal circumstances. A decreased interval may indicate rotator cuff tear, while a coracohumeral distance of less than 11 mm in medial rotation suggests impingement and rotator cuff pathology.
Coracoclavicular Distance: The normal coracoclavicular interspace measures 1.1 to 1.3 cm. This measurement is important when evaluating acromioclavicular joint injuries using stress radiographs with 9 kg weights applied to each hand.
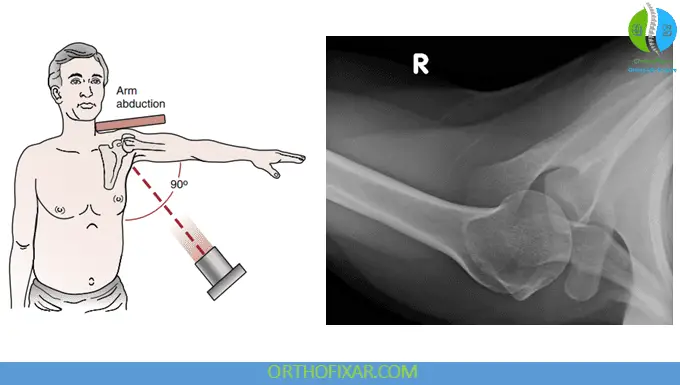
Axillary Lateral View
The axillary lateral view is used to visualize the relationship between the humeral head and glenoid, making it the gold standard for diagnosing anterior and posterior glenohumeral dislocations. This view requires the patient to abduct the arm 70° to 90°, which may limit its use in patients with acute injuries or significant pain.
Clinical Applications
This projection excels at demonstrating the coracohumeral distance and is particularly valuable for identifying avulsion fractures of the glenoid or Hill-Sachs lesions. The axillary view provides the best visualization of the acromioclavicular joint and allows assessment of calcifications in the subscapularis, infraspinatus, or teres minor muscles. Dynamic axillary views can be employed to evaluate horizontal instability of the acromioclavicular joint.
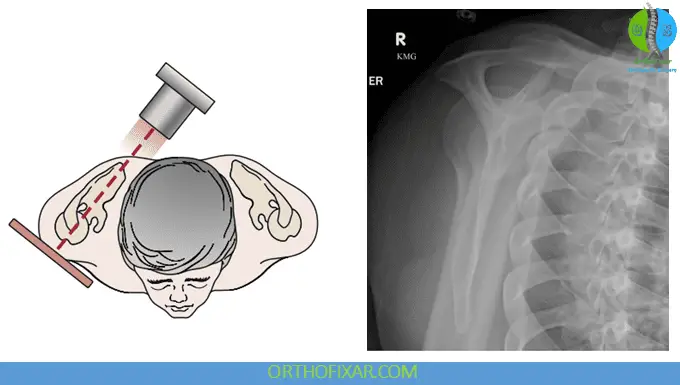
Trans-scapular (Y) Lateral (Outlet) View
The trans-scapular lateral view, also known as the Y view or outlet view, represents the true lateral projection of the scapula. This view is invaluable for assessing the position of the humerus relative to the glenoid and evaluating the morphology of both the acromion and coracoid processes.
Clinical Significance
The outlet view is used to determine the coracoacromial outlet shape and its contribution to impingement syndrome. By visualizing the subacromial space from a lateral perspective, clinicians can better understand the mechanical factors contributing to rotator cuff pathology.
Specialized Views for Specific Pathology
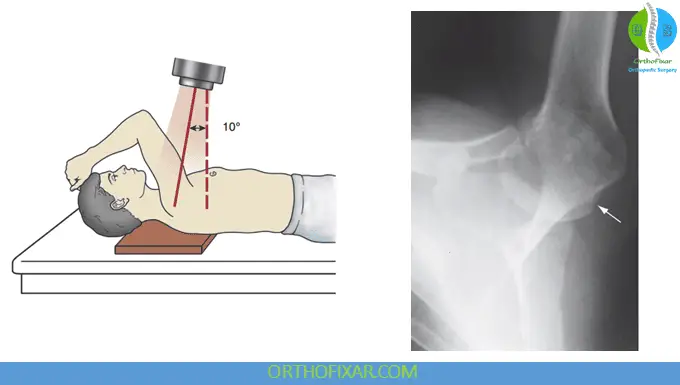
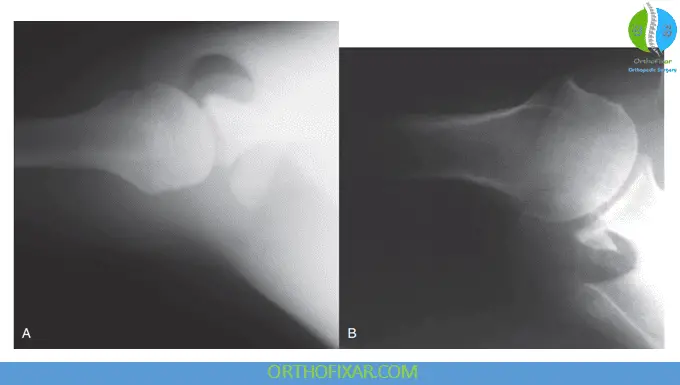
Stryker Notch View
This specialized projection requires the patient to lie supine with the arm forward flexed, and the hand positioned on top of the head, with the radiograph centered on the coracoid process. The Stryker notch view is specifically designed to assess coracoid fractures, Hill-Sachs lesions, and Bankart lesions with enhanced sensitivity.
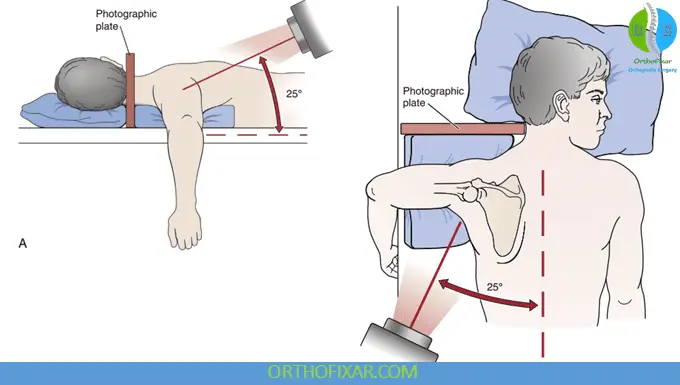
West Point View
This view is performed with the patient in a prone position, the West Point view provides excellent visualization of the glenoid to delineate fractures and bony abnormalities of the anterior glenoid rim. This view is particularly useful for evaluating chronic instability patterns and identifying subtle bony lesions.
Arch View
This lateral projection focuses on determining the width and height of the subacromial arch, helping clinicians classify the type of acromial arch and its potential contribution to impingement syndrome.

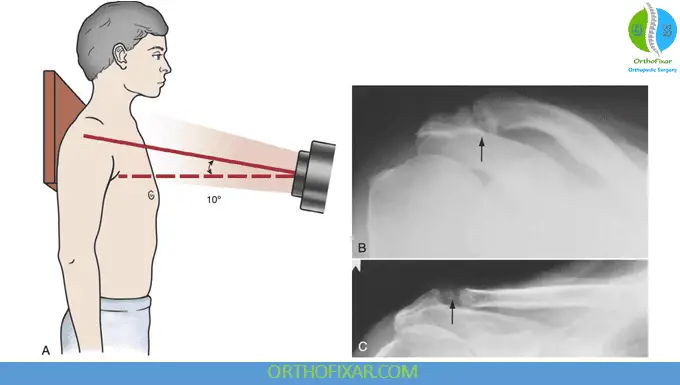
Zanca View
The Zanca view is used to diagnose the posterior acromioclavicular joint dislocations by measuring the distance between the acromion and clavicle ends. The AC width index (ACI) is calculated using the formula:
ACI = (Width of injured side – width of normal side) × 100% / width of normal (uninjured) side
An index of ≥60% indicates posterior acromioclavicular dislocation. This view also effectively demonstrates degenerative changes within the acromioclavicular joint.
Clinical Integration and Best Practices
When interpreting shoulder X-ray views, it’s essential to approach each case systematically, evaluating all relevant anatomical structures and their relationships. Begin with the AP view to establish baseline anatomy and identify obvious pathology, then use specialized views to confirm suspected diagnoses or evaluate specific clinical concerns.
Remember that plain radiographs have limitations, and advanced imaging such as MRI or CT may be necessary for complete evaluation of soft tissue injuries, subtle fractures, or complex pathology. However, mastering the interpretation of these fundamental shoulder X-ray views provides the foundation for accurate diagnosis and appropriate treatment planning in shoulder pathology.
References & More
- Anderson MW, Brennan C, Mittal A. Imaging evaluation of the rotator cuff. Clin Sports Med. 2012;31:605–631. Pubmed
- Tauber M, Koller H, Hitzl W, et al. Dynamic radiographic evaluation of horizontal instability in acute acromioclavicular joint dislocations. Am J Sports Med. 2010;38:1188–1195. Pubmed
- Pavlov H, Warren RF, Weiss CB, et al. The roentgenographic evaluation of anterior shoulder instability. Clin Orthop. 1985;194:153–158. Pubmed
- Engebretsen L, Craig EV. Radiologic features of shoulder instability. Clin Orthop. 1993;291:29–44. Pubmed
- Vaisman A, Villalon Montenegro IE, Tuca De Diego MJ, Valderrama Ronco JV. A novel radiographic index for the diagnosis of posterior acromioclavicular joint dislocations. Am J Sports Med. 2014;42(1):112–116. Pubmed
- Orthopedic Physical Assessment by David J. Magee, 7th Edition.

Closed.