The hip joint X-ray is an essential diagnostic tool for evaluating pain, trauma, deformities, and developmental conditions affecting the hip and pelvis. Normally, standard radiographic evaluation includes anteroposterior (AP) and axial (frog-leg) views. Additional views may be required depending on the suspected pathology.
Common Hip X-Ray Views
Depending on the clinical scenario, several Hip X-Ray views may be used:
- Anteroposterior (AP) view of the hip
- Lateral view (cross-table) – affected hip only
- Lateral axial (“frog-leg”) view
- Anteroposterior view of both hips and pelvis
- Anteroposterior oblique view
- AP internal (medial) rotation view
These hip x-ray views help assess joint alignment, femoral head coverage, acetabular orientation, bone integrity, and subtle deformities such as femoroacetabular impingement (FAI) or dysplasia.
See Also: Hip Joint Anatomy
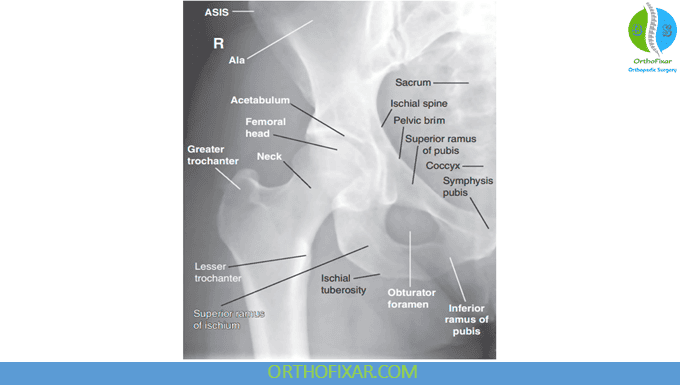
AP Hip X-Ray
When reviewing an AP radiograph of the pelvis or hip, the following details should be carefully examined:
1. Neck–shaft angle, femoral head coverage, and head–teardrop distance
Begin by assessing the relationship between the femoral head and neck. An abnormal head–neck offset—characterized by loss of femoral head sphericity and flattening of the normal concave lateral femoral neck—produces the classic pistol-grip deformity. This radiographic sign is commonly associated with femoroacetabular impingement (FAI), femoral head dysplasia, slipped capital femoral epiphysis (SCFE), and Legg–Calvé–Perthes disease.
2. Joint spaces and pelvic reference lines
Evaluate the width and symmetry of the joint spaces, as well as key pelvic lines and anatomic landmarks.
3. Evidence of bone disease
Look for signs of conditions such as Legg–Calvé–Perthes disease, bony cysts, or tumors. In Perthes disease, a prominent ischial spine may indicate acetabular retroversion.
4. Neck–shaft angle
Determine whether the neck–shaft angle is normal or demonstrates coxa vara or coxa valga, as these deformities significantly affect hip biomechanics.
5. Femoral head shape
A normal femoral head is round and spherical. Alterations in shape may occur in DDH, Perthes disease, SCFE, or FAI.
6. Obturator foramen symmetry
Both obturator foramina should appear symmetrical; asymmetry usually indicates pelvic rotation on the radiograph.
7. Symphysis pubis–coccyx distance and acetabular depth
The distance from the symphysis pubis to the tip of the coccyx should measure 1–3 cm.
8. Assess for coxa profunda (excessive acetabular depth) or coxa protrusio (medial displacement of the femoral head beyond the ischiofemoral line).
9. Protrusio acetabuli
Protrusio is present when the medial femoral head lies medial to the ilioischial line, indicating excessive acetabular coverage.
10. Acetabular version
Determine whether the acetabulum is anteverted (normal) or retroverted.
Retroversion is suggested by:
- Crossover sign (figure-eight sign) – anterior acetabular rim crosses over the posterior rim.
- Posterior wall sign – posterior acetabular wall lies medial to the femoral head center, indicating decreased posterior coverage.
11. Femoral head position
The femoral head should lie less than 10 mm from the ilioischial line. Increased distance may indicate subluxation or dysplasia.
12. Joint congruency
Evaluate whether the femoral head and acetabulum match in contour, as incongruency suggests dysplasia or degenerative changes.
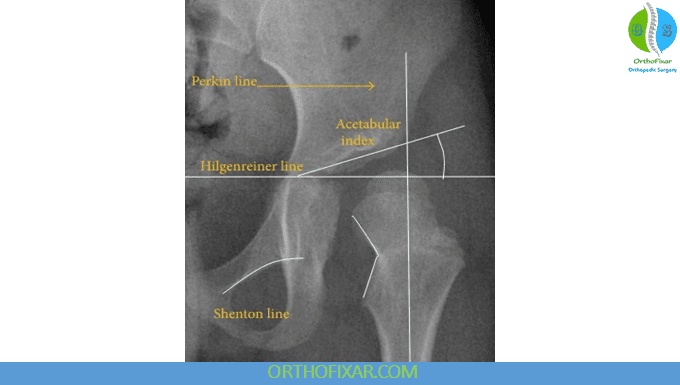
13. Acetabular index (Hilgenreiner angle / Sharp angle)
Assess acetabular development, especially in pediatric patients.
- Normal values: < 30° in newborns, < 20° by age 2, and < 36° in adults.
Higher angles indicate acetabular dysplasia, and the steeper the roof, the less stable the femoral head.
14. Femoral head extrusion index
Normally approximately 25%. Higher values indicate lateral uncovering and possible instability.
15. Signs of osteoarthritis
Check for:
- Joint-space narrowing
- Osteophyte formation
- Subchondral sclerosis
- Subchondral cysts
The Kellgren–Lawrence grading scale is commonly used to classify severity.
16. Shenton’s line
This smooth arc follows the medial femoral neck and inferior pubic ramus. A broken Shenton’s line suggests femoral neck fracture, dislocation, or SCFE.
17. Acetabular (Tönnis) angle
Normal in adults: 0°–10°.
Angles >10° indicate acetabular dysplasia.
18. Lateral center-edge angle (LCEA)
Normally > 25° on AP view.
Values < 25° indicate insufficient femoral head coverage or dysplasia.
19. Evidence of femoroacetabular impingement (FAI)
Look for cam or pincer morphology or combined deformities.
20. Fractures or dislocations
Assess for disruptions of the femoral neck, acetabulum, or pelvic ring. Pelvic ring disruption signifies a severe injury.
21. Pelvic distortion
Look for counterrotation of the ilia relative to the sacrum, which may affect measurements and alignment.
22. Hilgenreiner’s and Perkins’ lines (pediatric dysplasia evaluation)
- Hilgenreiner’s line: horizontal line through the inferomedial ilium.
- Perkins’ line: vertical line through the superolateral acetabular edge.
In normal development, the femoral head ossification center lies in the inferomedial quadrant.
If the ossification center is in the superolateral quadrant, the finding suggests dislocation or DDH. In newborns, the ossification center may not yet be visible.
23. “Sagging rope” sign
Seen in severe Legg–Calvé–Perthes disease. It represents physeal damage with pronounced metaphyseal reaction and indicates advanced disease.
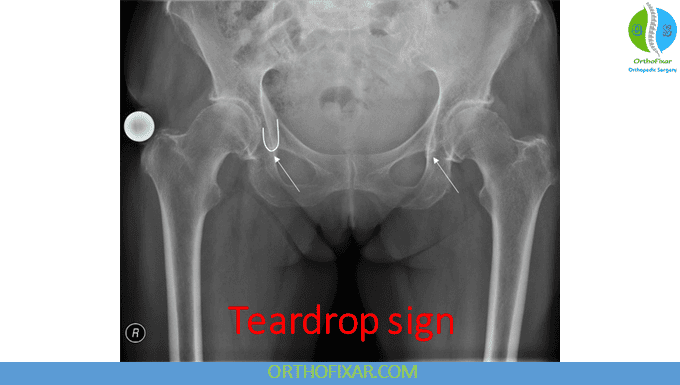
24. “Teardrop” sign
Upward migration of the femoral head relative to the pelvis—often due to degenerative changes such as advanced osteoarthritis—can be identified using the teardrop sign. The teardrop structure appears at the base of the pubic bone, extending vertically downward and terminating in a rounded “teardrop” shape.
To assess femoral head migration, the x-ray beam must be centered correctly over the pelvis. A horizontal line is drawn between the two teardrops and extended toward both femoral heads. Measuring the distance between each teardrop and its corresponding femoral head helps identify asymmetry. A difference greater than 10 mm between sides indicates significant femoral head migration. Serial radiographs often demonstrate progressive displacement over time.
25. “Head-at-Risk” Signs in Legg–Calvé–Perthes Disease
When evaluating patients with Legg–Calvé–Perthes disease, several radiologic features on the AP pelvis view may indicate a poor prognosis. These include:
a. Cage sign – a small, osteoporotic, translucent segment along the lateral epiphysis.
b. Lateral calcification – calcification adjacent to the epiphysis, suggesting collapse.
c. Lateral subluxation – increased inferomedial joint space indicating displacement of the femoral head.
d. Horizontal epiphyseal plate – the growth plate appears abnormally horizontal.
e. Metaphyseal reaction – reactive changes in the metaphysis.
Patients who exhibit three or more of these findings generally have a poor prognosis and often require surgical management.
26. Radiographic Signs of Slipped Capital Femoral Epiphysis (SCFE)
In SCFE, several characteristic x-ray findings may be present:
a. Widening of the epiphyseal plate.
b. Lipping or stepping deformity, especially evident on lateral projections.
c. Loss of normal intersection – the line along the superior femoral neck fails to intersect the displaced overhanging epiphysis.
d. Interrupted Shenton’s line – this smooth curve becomes discontinuous, also seen in hip dislocation or subluxation.
Although SCFE commonly results in coxa vara, other conditions such as fractures or congenital deformities may produce a similar appearance.
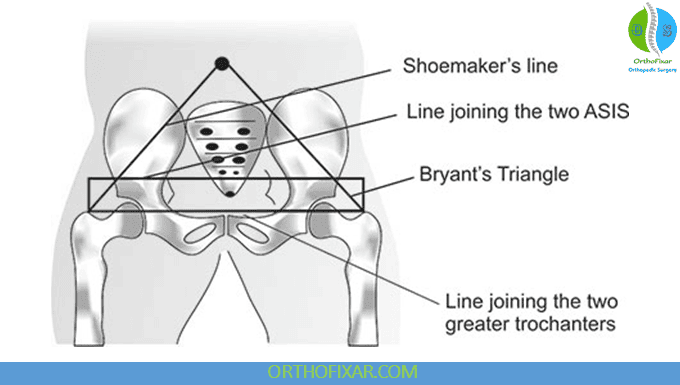
27. Shoemaker’s Line
When a line is drawn from each greater trochanter to the ipsilateral anterior superior iliac spine (ASIS), the two lines should meet at or above the umbilicus.
If the lines intersect below the umbilicus or asymmetrically, this suggests:
- Femoral neck fracture
- Superior displacement of a femur (e.g., dislocation)
- Malalignment of the pelvis or proximal femur
28. Lateral Coverage Index (LCI)
The LCI is useful in assessing hip stability and dysplasia. It is calculated as:
LCI = Center-edge (CE) angle – Acetabular inclination
Higher LCI values correlate with more stable hips and are associated with fewer ligamentum teres tears.
29. Acetabular Coverage of the Femoral Head
Acetabular coverage can be assessed through several measurements:
- Lateral center-edge (LCE) angle
- Anterior center-edge angle
- Acetabular inclination (Tönnis angle)
- Acetabular index
A normal LCE angle is ≥ 25°. Values below 25° indicate acetabular dysplasia, reflecting inadequate lateral coverage.
30. Radiographic Features of Femoroacetabular Impingement (FAI)
Cam-type FAI may be diagnosed by:
- Alpha angle > 57°
- Pistol-grip deformity
- Tönnis angle < 0°
- Femoral head–neck offset < 8 mm
- Offset ratio or triangular index abnormalities
Pincer-type FAI may be identified by:
- Crossover sign
- Posterior wall sign
- LCE angle > 40°
- Ischial spine sign
- Coxa profunda
31. Acetabular Orientation and Hip Stability
Acetabular version plays a critical role in hip stability:
- A retroverted acetabulum may predispose to posterior instability.
- An anteverted acetabulum or anteverted femoral neck may predispose to anterior instability.
Retroversion is suggested by the posterior wall sign and/or ischial spine sign.
32. Osteopenia on Plain Radiographs
It is important to note that osteopenia is not normally visible on x-rays until approximately 40% of bone mineral density has been lost.
33. Radiographic Signs of Hip Joint Effusion
Joint effusion may present with:
a. Lateral subluxation of the femoral head, widening the joint space (common in juvenile rheumatoid arthritis).
b. Absence of the vacuum phenomenon during traction radiographs—in a normal hip, negative intraarticular pressure appears as a radiolucent crescent; this disappears when effusion is present.
c. Subchondral demineralization, appearing as loss of the sharp, dense subchondral line of the femoral head.
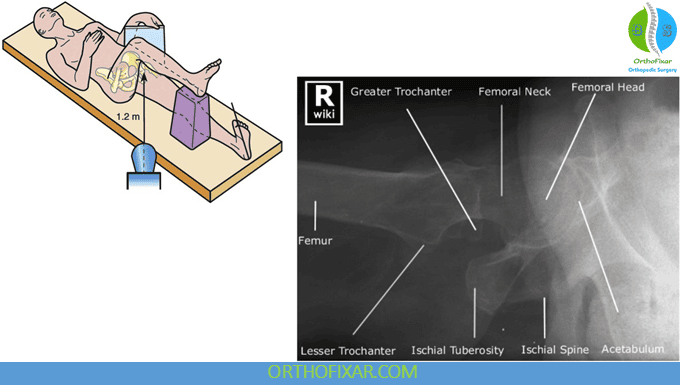
Cross-Table Lateral Hip X-Ray
The cross-table lateral radiograph provides an axial projection of the proximal femur and is particularly useful when evaluating for femoroacetabular impingement (FAI), especially the cam-type variant. This projection allows measurement of the head–neck offset ratio.
To calculate the head–neck offset ratio:
- A line is drawn along the long axis of the femoral neck.
- Perpendicular lines are then drawn to determine the distance between the most anterior aspect of the femoral head and the most anterior aspect of the femoral neck.
- The ratio is obtained by dividing this anterior offset by the diameter of the femoral head.
A head–neck offset ratio < 0.17 is considered abnormal and suggests a cam deformity, which may contribute to FAI.
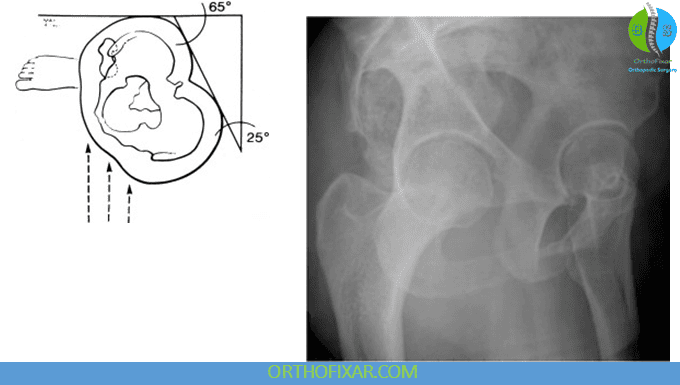
False-Profile Hip X-Ray
The false-profile view is an oblique (65°) standing radiograph used to assess anterior acetabular coverage of the femoral head. It is the standard view for calculating the anterior center-edge (CE) angle.
Measurement steps:
- A vertical line is drawn through the center of the femoral head.
- A second line is drawn from the most anterior point of the acetabular sourcil (“eyebrow”) to the femoral head center.
- The angle between these two lines is the anterior CE angle.
Interpretation:
- < 20° → structural instability of the hip
- Normal → typically > 20°
This measurement is particularly important when evaluating dysplasia, instability, or pre-arthritic structural abnormalities in young adults.
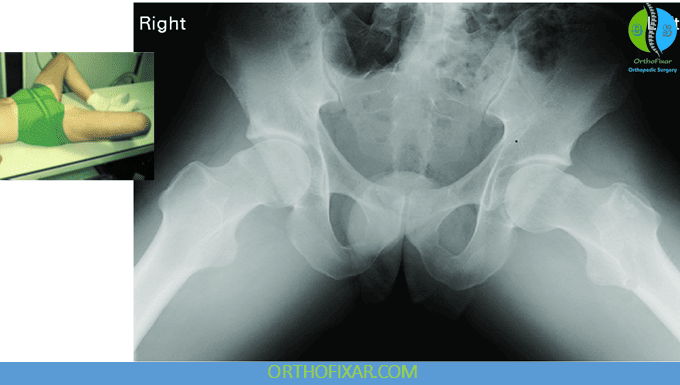
Lateral (Axial “Frog-Leg”) View
The frog-leg lateral hip x-ray is obtained with the patient supine and the hips placed in flexion, abduction, and lateral rotation. This positioning produces a true lateral view of both the femoral head and neck.
Clinical applications:
- Avascular necrosis (AVN): Early contour irregularities or sclerosis may be detected.
- Slipped Capital Femoral Epiphysis (SCFE):
- The frog-leg lateral view is often the first projection in which the slip becomes visible, making it essential in suspected SCFE.
- Posterior and inferior displacement of the epiphysis relative to the metaphysis can be appreciated.
- Head-neck offset deformity: Used to assess morphology relevant to cam-type FAI.
- Pelvic distortion or rotational malalignment can also be detected.
This view therefore plays a critical role in early detection of both growth-related hip disease (e.g., SCFE, Perthes) and structural abnormalities contributing to impingement or instability.
References & More
- Clohisy JC, Carlisle JC, Beaulé PE, et al. A systematic approach to the plain radiographic evaluation of the young adult hip. J Bone Joint Surg Am. 2008;90:47–66. PubMed
- Lee WA, Saroki AJ, Loken S, et al. Radiographic identification of arthroscopically relevant proximal femoral structures. Am J Sports Med. 2015;44(1):60–66. PubMed
- Zaltz I, Kelly BT, Hetsroni I, Bedi A. The crossover sign overestimates acetabular retroversion. Clin Orthop Relat Res. 2013;471(8):2463–2470.
- Kappe T, Kocak T, Neuerburg C, et al. Reliability of radiographic signs for acetabular retroversion. Int Orthop. 2011;35(6):817–821
- Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494–502.
- Llopis E, Higueras V, Vano M, Altonaga JR. Anatomic and radiographic evaluation of the hip. Eur J Radiol. 2012;81(12):3727–3736.
- Wong TY, Jesse MK, Jensen A, et al. Upsloping lateral sourcil: a radiographic finding of hip instability. J Hip Preserv Surg. 2018;5(4):435–442.
- Bigg-Wither G, Kelly P. Diagnostic imaging in musculoskeletal physiotherapy. In: Refshauge K, Gass E, eds. Musculoskeletal Physiotherapy. Oxford: Butterworth Heinemann; 1995
- Orthopedic Physical Assessment by David J. Magee, 7th Edition.

Closed.