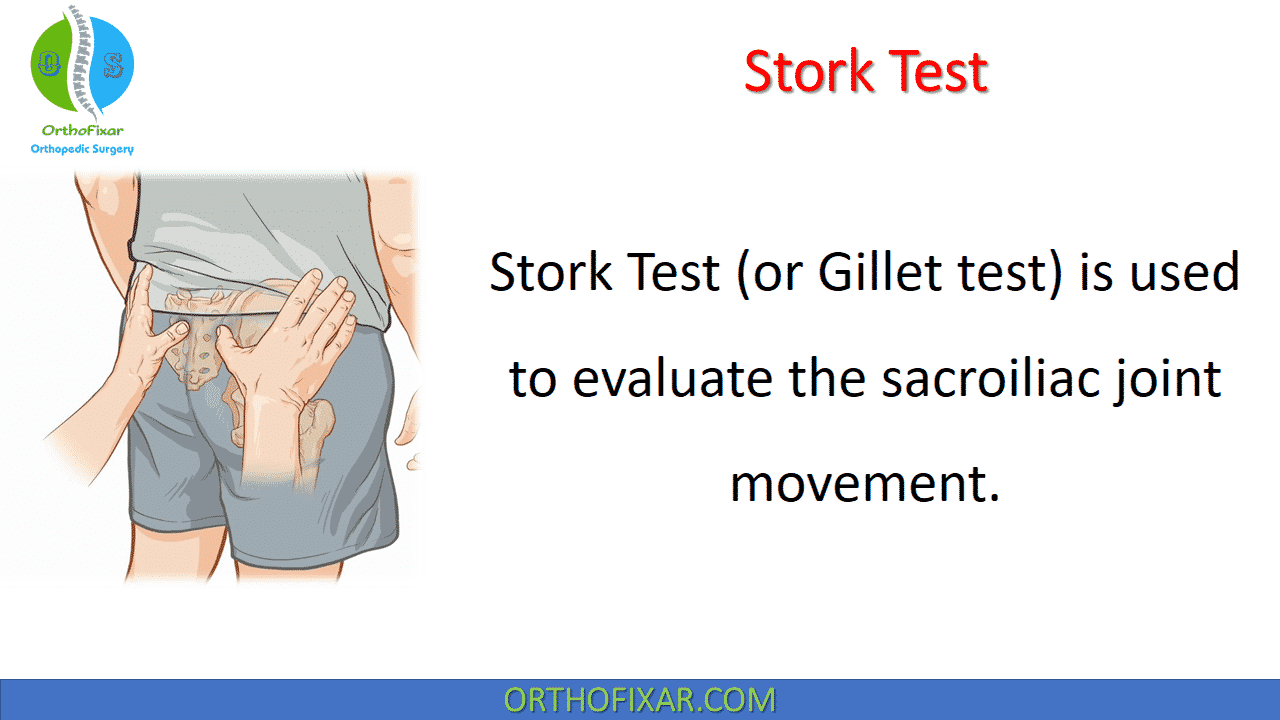
The Stork Test, also known as the Gillet Test or Ipsilateral Posterior Rotation Test, is commonly used to assess sacroiliac joint (SIJ) mobility dysfunction. The SI joint normally exhibits very small motion (usually 2 mm or less), and patient-specific bony anatomy can vary significantly, making subtle mobility changes difficult to detect.
Despite this limitation, the Stork/Gillet test remains widely taught because it offers insights into innominate rotation, weight-transfer mechanics, and muscle activation patterns.
How do you perform the Stork Test?
With patient standing, the examiner palpates the following landmarks:
- L5 spinous process and posterior superior iliac spine (PSIS),
- S1 tubercle and PSIS,
- S3 tubercle and PSIS,
- Sacral apex and posteromedial margin of the ischium.
Patient is instructed to raise the ipsilateral leg of the side of palpation. The test is then repeated on the other side and compared bilaterally.
See Also: Patrick Test | FABER Test
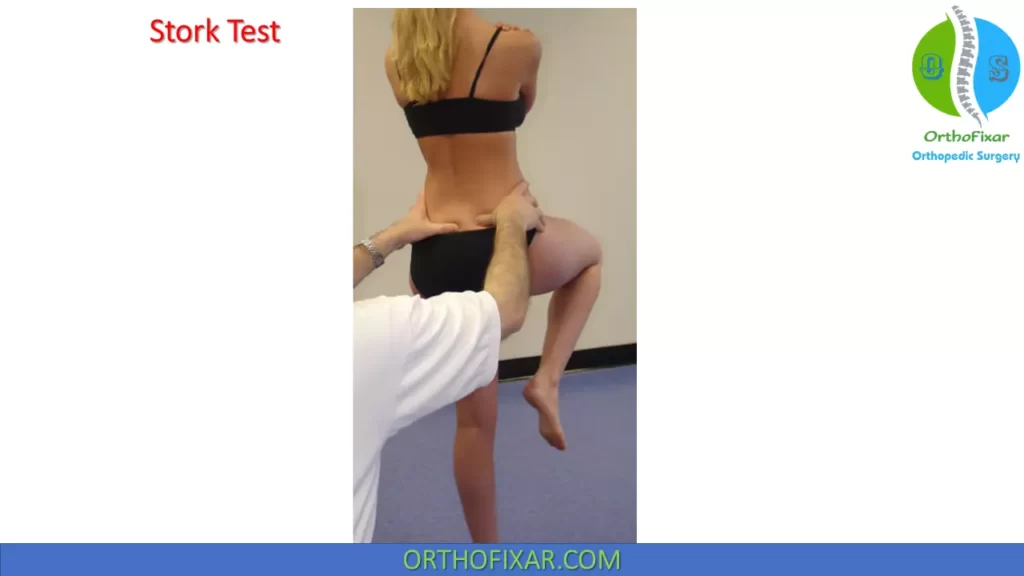
Another way to perform the Stork Test is as following:
With patient standing with feet spread 12 inches apart, examiner palpates the S2 spinous process with one thumb and the posterior superior iliac spine (PSIS) with the other. The patient then flexes the hip and knee on the side being tested. The test is considered positive if the PSIS fails to move in a posteroinferior direction relative to S2.

What does a positive Stork Test mean?
Stork Test is positive if the lateral landmark posterior superior iliac spine (PSIS) fails to move posteroinferiorly with respect to medial landmark (L5, S1, S3 or Sacral apex).
This suggests:
- SI joint hypomobility
- Sacroiliac “block” or fixation
- Altered posterior innominate rotation mechanics
Accuracy
A study on 85 consecutive patients with low back pain referred for sacroiliac joint blocks, found that the sensitivity and specificity of Stork Test was:
- Sensitivity: 47%
- Specificity: 64 %
In this study, 90% relief with injection of local anesthetics into sacroiliac joint.
Both inter- and intra-examiner reliability data showed high mean percentages of agreement (85.3% and 89.2%, respectively). The intra-examiner reliability data suggests that the Gillet test is clinically useful for a single examiner in assessing the sacroiliac joint for mobility dysfunction, especially at upper sacroiliac contact points.
Another study on 274 patients being treated for low back pain or another condition not related to the low back found that the sensitivity and specificity was 8% and 93% respectively.
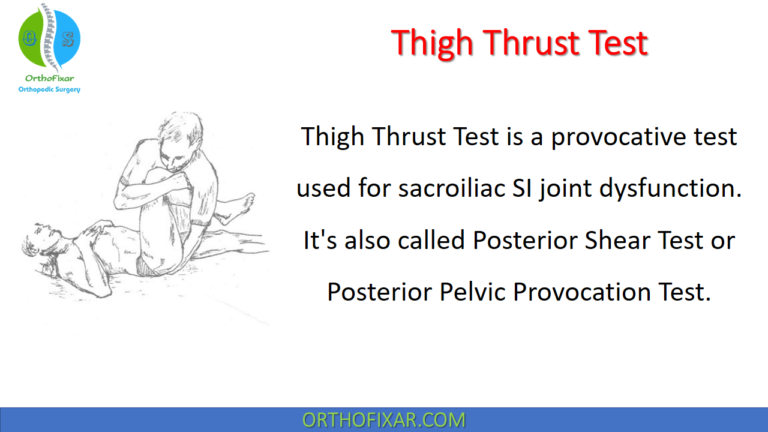
Selective tissue tests for the SI joint either try to detect asymmetry or aberrant movement patterns or provoke symptoms by stressing the joint. Provocation tests, such as Gaenslen’s test (or Patrick’s test), sacral thrust test, and thigh thrust test are more reliable and valid than tests that attempt to detect differences in movement or position, such as the Gillet test.
See Also:
References
- Carmichael JP. Inter- and intra-examiner reliability of palpation for sacroiliac joint dysfunction. J Manipulative Physiol Ther. 1987 Aug;10(4):164-71. PMID: 3655566.
- Dreyfuss P, Michaelsen M, Pauza K, McLarty J, Bogduk N. The value of medical history and physical examination in diagnosing sacroiliac joint pain. Spine (Phila Pa 1976). 1996 Nov 15;21(22):2594-602. doi: 10.1097/00007632-199611150-00009. PMID: 8961447.
- Levangie PK. Four clinical tests of sacroiliac joint dysfunction: the association of test results with innominate torsion among patients with and without low back pain. Phys Ther. 1999 Nov;79(11):1043-57. PMID: 10534797.
- Potter, NA, and Rothstein, JM: Intertester reliability for selected clinical tests of the sacroiliac joint. Phys Ther, 65:1671, 1985.
- Laslett, M, and Williams, M: The reliability of selected pain provocation tests for sacroiliac joint pathology. Spine, 19:1243, 1994.
- Robinson, HS, et al: The reliability of selected motion- and pain provocation tests for the sacroiliac joint. Man Ther, 12:72, 2009.
- Netter’s Orthopaedic Clinical Examination An Evidence-Based Approach 3rd Edition Book.