The posterior tibial pulse (PT pulse) is a key component of the lower limb vascular examination. Accurate palpation helps clinicians assess distal perfusion, detect peripheral arterial disease (PAD), and identify acute arterial emergencies.
What is the Posterior Tibial Pulse?
The posterior tibial pulse reflects blood flow through the posterior tibial artery, a terminal branch of the popliteal artery. It supplies the plantar aspect of the foot and is one of the two primary distal pulses in the lower limb (the other being the dorsalis pedis pulse).
Palpation of the PT pulse is essential in:
- Peripheral arterial disease (PAD) screening
- Diabetic foot assessments
- Post-trauma vascular evaluation
- Acute limb ischemia diagnosis
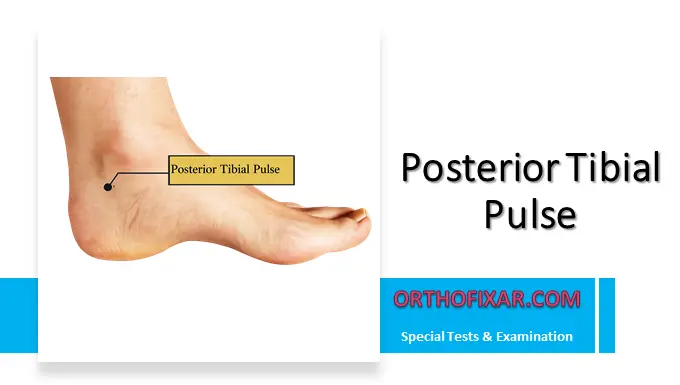
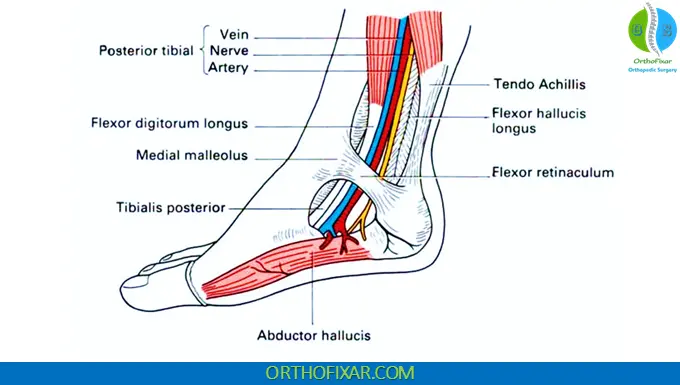
Posterior Tibial Pulse Location
The PT pulse is palpated behind and slightly below the medial malleolus of the ankle.
Anatomical Landmark
- Medial malleolus (distal tibia prominence)
- Posterior and inferior to this bony landmark
- Between the medial malleolus and the Achilles tendon
This location places the artery in the tarsal tunnel, where it runs superficially enough to be palpated.
See Also: Ankle Anatomy
Step-by-Step: How to Palpate the Posterior Tibial Pulse
1. Position the Patient
- The patient should be supine or seated comfortably.
- The ankle should be slightly relaxed.
- Avoid excessive dorsiflexion or plantarflexion.
2. Hand Placement
- Curve your fingers behind and slightly below the medial malleolus.
- Use the pads of your index and middle fingers.
- Do NOT use your thumb (it has its own pulse).
3. Apply Gentle Pressure
- Press inward and slightly upward toward the tibia.
- Avoid excessive force, which may occlude the artery.
4. Assess the Pulse
Evaluate:
- Presence or absence
- Symmetry (compare both sides)
- Amplitude (0–3+ scale commonly used)
- Rhythm

Why the Posterior Tibial Pulse May Be Difficult to Feel
The PT pulse can be challenging to palpate in:
- Obese patients
- Fat or edematous ankles
- Patients with severe peripheral arterial disease
- Advanced atherosclerosis
If the pulse is not palpable, consider:
- Using Doppler ultrasound
- Comparing with dorsalis pedis pulse
- Assessing capillary refill and skin temperature
Clinical Significance: Acute Arterial Occlusion
One of the most critical clinical scenarios involving the posterior tibial pulse is acute arterial occlusion due to embolism or thrombosis.
Classic Symptoms
Acute occlusion causes:
- Severe pain
- Numbness
- Tingling
- Cold limb
- Pale skin
- Absent distal pulses
These findings are consistent with acute limb ischemia, often summarized as the “6 Ps”:
- Pain
- Pallor
- Pulselessness
- Paresthesia
- Paralysis
- Poikilothermia
This is a vascular emergency.
Immediate Action
If suspected:
- Urgent vascular referral
- Emergency imaging (e.g., duplex ultrasound or CT angiography)
- Immediate revascularization may be required
Delay can result in tissue necrosis or limb loss.
Guidelines from the Society for Vascular Surgery emphasize rapid diagnosis and intervention in cases of suspected acute limb ischemia.
Posterior Tibial Pulse vs Dorsalis Pedis Pulse
Both pulses are assessed together in a comprehensive lower limb vascular exam:
| Feature | Posterior Tibial Pulse | Dorsalis Pedis Pulse |
|---|---|---|
| Location | Behind & below medial malleolus | Dorsum of foot |
| Artery | Posterior tibial artery | Dorsalis pedis artery |
| Clinical Use | PAD, acute ischemia | PAD screening |
Absence of both pulses increases suspicion of significant arterial compromise.
See Also: Radial Artery Pulse Location
When to Document Abnormal Findings
Document carefully if you note:
- Absent pulse (0)
- Diminished pulse (1+)
- Asymmetry between limbs
- Signs of ischemia
- Skin color changes
- Ulceration or delayed capillary refill
Accurate documentation supports early diagnosis of vascular disease.
Key Takeaways
- The posterior tibial pulse is palpated behind and slightly below the medial malleolus.
- It may be difficult to feel in fat or edematous ankles.
- Absence of the pulse with pain, pallor, coldness, and numbness suggests acute arterial occlusion.
- Acute limb ischemia requires emergency treatment.
- Always compare bilaterally and document findings clearly.
FAQ
Where exactly is the posterior tibial pulse located?
The posterior tibial pulse is palpated behind and slightly below the medial malleolus (the inner ankle bone). It lies between the medial malleolus and the Achilles tendon, in the region of the tarsal tunnel.
How do you properly palpate the posterior tibial pulse?
– Position the patient comfortably with the foot relaxed.
– Curve your index and middle fingers behind and slightly inferior to the medial malleolus.
– Apply gentle, steady pressure inward toward the tibia.
– Avoid using your thumb to prevent feeling your own pulse.
– Compare both sides for symmetry.
What does it mean if the posterior tibial pulse is absent?
An absent pulse may indicate:
– Peripheral arterial disease (PAD)
– Advanced atherosclerosis
– Acute arterial occlusion
– Severe edema or obesity masking the pulse
If absent, assess the dorsalis pedis pulse and consider Doppler evaluation. Persistent absence with ischemic symptoms requires urgent evaluation.
Why can the posterior tibial pulse be difficult to feel?
The pulse may be hard to detect in:
– Fat or edematous ankles
– Obese patients
– Patients with significant vascular disease
– Severe arterial calcification
In such cases, handheld Doppler ultrasound improves detection.
What are the signs of acute arterial occlusion?
Acute arterial occlusion from embolism or thrombosis typically presents with:
– Sudden severe pain
– Numbness or tingling (paresthesia)
– Cold limb
– Pale skin
– Absent distal pulses
This condition corresponds to acute limb ischemia and requires emergency treatment, as emphasized by the Society for Vascular Surgery.
Is the posterior tibial pulse always palpable in healthy individuals?
Not always. Although most healthy individuals have a palpable PT pulse, anatomical variation exists. However, bilateral absence is uncommon and should raise suspicion for vascular pathology, especially in patients with diabetes, smoking history, or cardiovascular disease risk factors.
What grading scale is used to document the posterior tibial pulse?
Clinicians commonly use a 0–3+ scale:
– 0 = Absent
– 1+ = Diminished
– 2+ = Normal
– 3+ = Bounding
Clear documentation supports accurate vascular assessment and follow-up.
Why is assessing the posterior tibial pulse important in diabetic patients?
Patients with diabetes are at increased risk for peripheral arterial disease and foot ulcers. Routine assessment of the posterior tibial pulse helps detect compromised perfusion early and reduce the risk of non-healing wounds and amputation. The American Diabetes Association recommends comprehensive foot examinations in diabetic care.
References & More
- Bickley, L. S., Szilagyi, P. G., Hoffman, R. M., & Soriano, R. P. (2021). Bates’ guide to physical examination and history taking, 12e.
- Zimmerman B, Williams D. Peripheral Pulse. [Updated 2025 Jul 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: Pubmed
- Lezak B, Wehrle CJ, Summers S. Anatomy, Bony Pelvis and Lower Limb: Posterior Tibial Artery. [Updated 2023 Jul 31]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: Pubmed