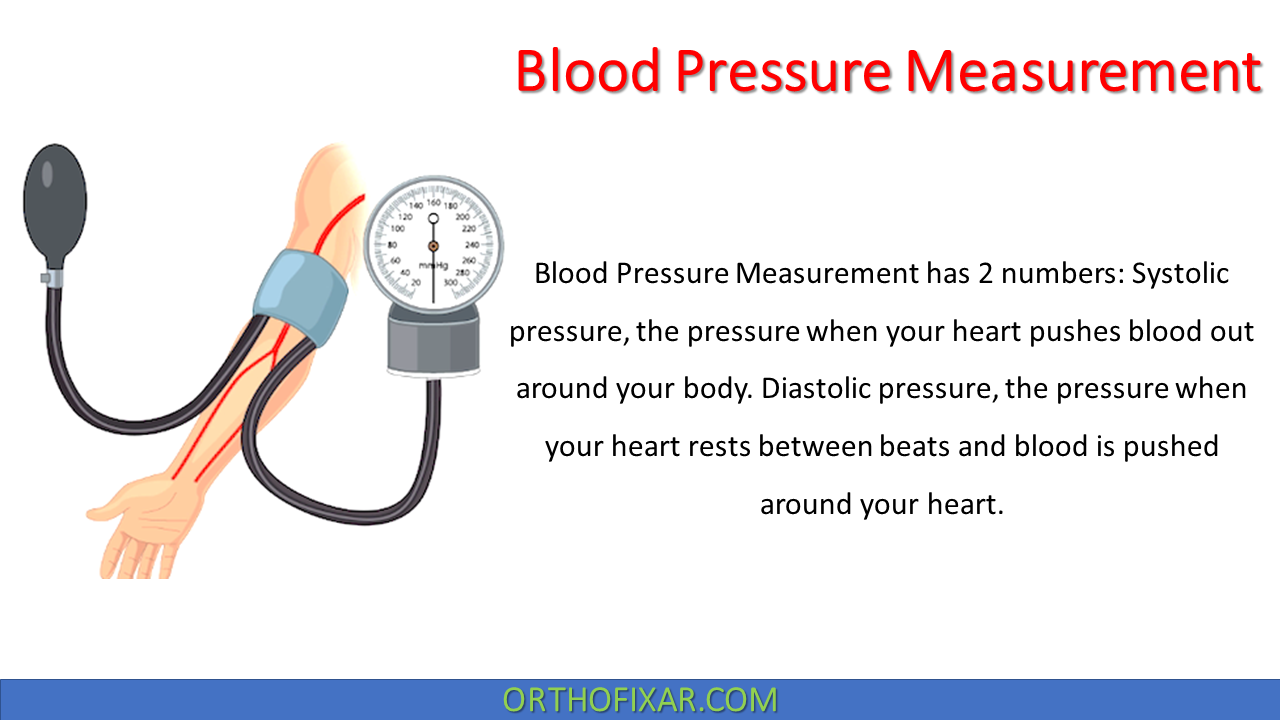
The Blood Pressure Measurement has two numbers, Systolic pressure and Diastolic pressure. The normal blood pressure is: 120 (Systolic ) / 80 (Diastolic ) mmHg. The blood pressure is measured in millimeters of mercury (mmHg).
Systolic pressure, the pressure when your heart pushes blood out around your body, where Diastolic pressure, the pressure when your heart rests between beats and blood is pushed around your heart.
Guidelines for Assessing Blood Pressure
Posture
Blood pressure obtained in the sitting position is recommended. The subject should sit quietly for 5 min, with the back supported and the arm supported at the level of the heart, before blood pressure is recorded.
Circumstances
- No caffeine during the hour preceding the reading.
- No smoking during the 30 min preceding the reading.
- A quiet, warm setting.
- The arm selected should be free of clothing, fistulas for dialysis, scars from brachial artery cutdowns, or lymphedema from axillary node dissection or radiation therapy
Equipment
- Cuff size: The bladder should encircle and cover two thirds of the length of the arm; if it does not, place the bladder over the brachial artery. If bladder is too short, misleading high readings may result.
- Manometer: Aneroid gauges should be calibrated every 6 months against a mercury manometer.
See Also: Balance Tests


Blood Pressure Measurement Technique
Position the Cuff and Arm: With the arm at heart level, center the inflatable bladder over the brachial artery. The lower border of the cuff should be about 2.5 cm above the antecubital crease. Secure the cuff snugly. Slightly flex the patient’s arm at the elbow.
Estimate the Systolic Pressure and Add 30 mm Hg: To decide how high to raise the cuff pressure, first estimate the systolic pressure by palpation. As you palpate the radial artery with the fingers of one hand, rapidly inflate the cuff until the radial pulse disappears. Read this pressure on the manometer and add 30 mm Hg. Using this sum for subsequent inflations prevents discomfort from unnecessarily high cuff pressures. It also avoids the occasional error caused by an auscultatory gap—a silent interval that may be present between the systolic and the diastolic pressures. Deflate the cuff promptly and completely and wait for 15 to 30 seconds.
Position the Stethoscope Bell Over the Brachial Artery: Now place the bell of a stethoscope lightly over the brachial artery, taking care to make an air seal with the full rim. Because the sounds to be heard, the Korotkoff sounds, are relatively low in pitch, they are generally better heard with the bell.
Identify the Systolic Blood Pressure: Inflate the cuff again rapidly to the target level, and then deflate the cuff slowly at a rate of about 2 to 3 mm Hg per second. Note the level when you hear the sounds of at least two consecutive beats. This is the systolic pressure.
Identify the Diastolic Blood Pressure: Continue to deflate the cuff slowly until the sounds become muffled and disappear. To confirm the disappearance point, listen as the pressure falls another 10 to 20 mm Hg. Then deflate the cuff rapidly to zero. The disappearance point, which is usually only a few mm Hg below the muffling point, provides the best estimate of diastolic pressure.
Average Two or More Readings: Read both the systolic and the diastolic levels to the nearest 2 mm Hg. Wait 2 or more minutes and repeat. Average your readings. If the first two readings differ by more than 5 mm Hg, take additional readings.
Measure Blood Pressure in Both Arms At Least Once: Normally, there may be a difference in pressure of 5 mm Hg and sometimes up to 10 mm Hg. Subsequent readings should be made on the arm with the higher pressure.

Home blood pressure monitoring (HBPM)
Home blood pressure monitoring is a self-monitoring tool that can be incorporated into the care for patients with hypertension and is recommended by major guidelines.
A growing body of evidence supports the benefits of patient home blood pressure monitoring compared with office-based monitoring: these include improved control of BP, diagnosis of white-coat hypertension and prediction of cardiovascular risk. Furthermore, Home blood pressure monitoring is cheaper and easier to perform than 24-hour ambulatory BP monitoring (ABPM).
National Institute for Clinical Excellence (NICE) guidelines for HBPM recommend that when using HBPM to confirm a diagnosis of hypertension it is necessary to ensure that:
- for each BP recording, two consecutive measurements are taken, at least 1 minute apart with the person seated;
- BP is recorded twice daily, ideally in the morning and evening; and
- BP recording continues for at least 4 days, ideally for 7 days.

Accuracy of Blood Pressure Measurements
The accuracy of blood pressure measurements varies according to how these measurements are taken. Office screening with manual and automated cuffs remains common, but elevated readings increasingly require confirmation with home and ambulatory monitoring. In its 2014 draft recommendations, the U.S. Preventive Services Task Force reported that 5% to 65% of elevated office blood pressures failed to be confirmed by ambulatory monitoring and recommended ambulatory blood pressure monitoring to confirm the diagnosis of hypertension.
Numerous studies show that ambulatory and home blood pressure monitoring are more predictive of cardiovascular disease and end organ damage than manual and automated measurements in the office.32 Automated ambulatory blood pressure monitoring measures blood pressure at preset intervals over 24 to 48 hours, usually every 15 to 20 minutes during the day and 30 to 60 minutes during the night. It is now considered the reference standard for confirming elevated office blood pressures
References & More
- George J, MacDonald T. Home Blood Pressure Monitoring. Eur Cardiol. 2015 Dec;10(2):95-101. doi: 10.15420/ecr.2015.10.2.95. PMID: 30310433; PMCID: PMC6159400. Pubmed
- https://www.nice.org.uk/guidance/cg127 NICE. Hypertension: Clinical management of primary hypertension in adults. Available at: (accessed 29 June 2015).
- Kaplan NM, Deveraux RB, Miller HS: Systemic hyperextension, Med Sci Sports Exerc 26:S269, 1994.
- McGrew CA: Clinical implications of the AHA preparticipation cardiovascular screening guidelines, Athletic Ther Today 5(4):55, 2000.
- Orthopedic Physical Assessment by David J. Magee, 7th Edition.