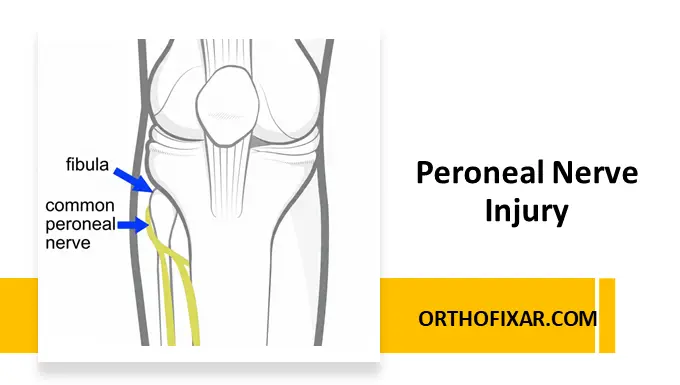
Peroneal nerve injury is a common peripheral neuropathy of the lower limb and an important cause of foot drop. Owing to its superficial course around the fibular neck, the peroneal (fibular) nerve is vulnerable to compression, traction, and trauma.
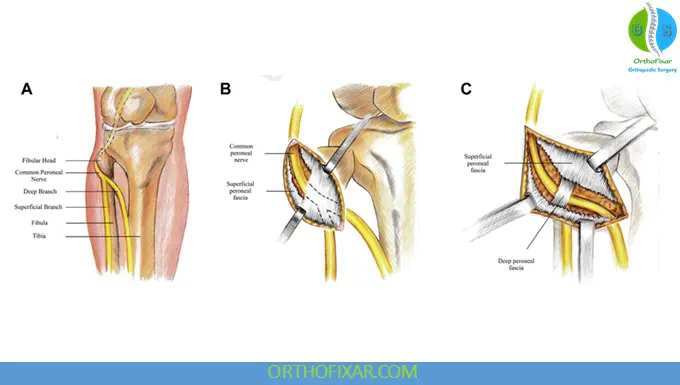
The common peroneal nerve is one of the two terminal branches of the sciatic nerve (roots L4–S2). It diverges from the tibial nerve at the superior angle of the popliteal fossa and courses laterally along the biceps femoris tendon. The nerve then winds superficially around the neck of the fibula, where it is most susceptible to injury, before dividing into:
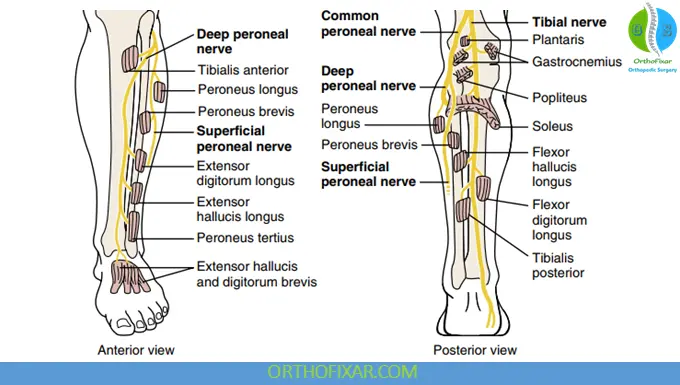
- Deep peroneal nerve
- Motor: tibialis anterior, extensor hallucis longus, extensor digitorum longus
- Sensory: first dorsal web space
- Superficial peroneal nerve
- Motor: peroneus longus and brevis
- Sensory: anterolateral leg and most of the dorsum of the foot
See Also: Common Peroneal Nerve Anatomy
Mechanisms & Etiology of Peroneal Nerve Injury
Peroneal nerve injury may result from several mechanisms:
- Compression
- Prolonged leg crossing
- Tight plaster casts or braces
- Prolonged squatting or kneeling
- Weight loss causing reduced protective fat padding
- Traction
- Varus stress to the knee
- Knee dislocation
- Pulling on the peroneus longus muscle in a lateral ankle sprain
- Direct trauma
- Fibular head or neck fractures
- Penetrating injuries
- Iatrogenic causes
- Knee surgery (e.g., total knee arthroplasty)
- Prolonged lithotomy position
- Systemic and metabolic causes
- Diabetes mellitus
- Peripheral neuropathies
Clinical Presentation
The hallmark feature of peroneal nerve injury is foot drop, resulting from paralysis of ankle dorsiflexors.
Motor Findings
- Weakness or paralysis of:
- Ankle dorsiflexion
- Toe extension
- Foot eversion (superficial branch involvement)
- Steppage gait due to inability to clear the foot during swing phase
Sensory Findings
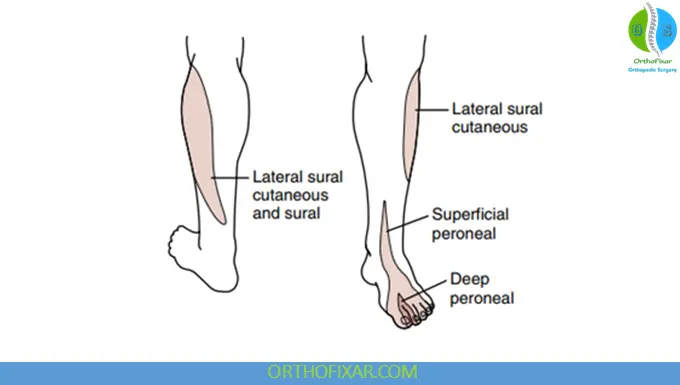
- Sensory loss or paresthesia over:
- Lateral aspect of the leg
- Dorsum of the foot
- First interdigital cleft (deep peroneal nerve)
Reflexes
- Typically preserved (helps differentiate from L5 radiculopathy)
Differential Diagnosis
Key conditions to consider include:
- L5 radiculopathy
- Sciatic nerve injury
- Motor neuron disease
- Central causes (e.g., stroke)
- Anterior compartment syndrome
Clinical distinction between peroneal neuropathy and L5 radiculopathy is critical; preservation of foot inversion (tibialis posterior, tibial nerve) favors peroneal nerve injury.
Diagnostic Evaluation
- Clinical examination remains the cornerstone of diagnosis.
- Electrodiagnostic studies
- Nerve conduction studies and electromyography help localize the lesion and assess severity.
- Imaging
- MRI or ultrasound may be used to identify compressive lesions, masses, or traumatic injury.
- Knee imaging is essential if trauma is suspected.
Management and Treatment
Peroneal nerve injury treatment depends on the cause, severity, and duration of the injury.
Conservative Treatment
- Removal of compressive factors
- Ankle-foot orthosis (AFO) to prevent foot drop
- Physical therapy focusing on:
- Strengthening preserved muscles
- Preventing contractures
- Neuropathic pain management if required
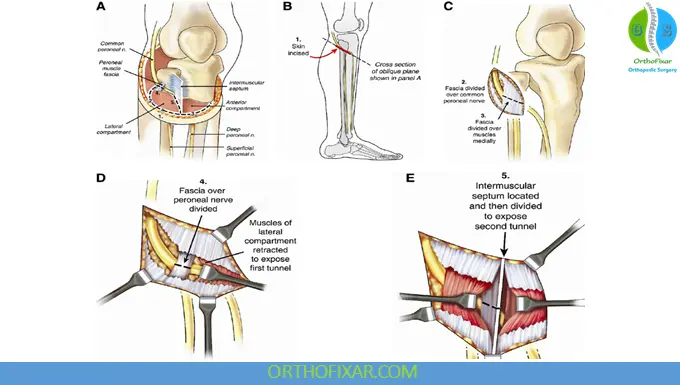
Surgical Intervention
Indications include:
- Persistent or progressive neurological deficit
- Identifiable compressive lesions
- Lack of recovery after 3–6 months of conservative management
Surgical options may include nerve decompression, neurolysis, or repair depending on the pathology.
Prognosis
The prognosis varies according to:
- Degree of nerve injury (neurapraxia vs. axonotmesis)
- Duration of compression
- Timeliness of intervention
Mild compression injuries often recover spontaneously, whereas severe traumatic injuries may result in incomplete recovery.
References & More
- Hyslop GH. Injuries of the deep and superficial peroneal nerves complicating ankle sprain. Am J Surg. 1941;51:436–438.
- Lezak B, Massel DH, Varacallo MA. Peroneal Nerve Injury. [Updated 2024 Feb 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: PubMed
- Sidey J. Weak ankles: a study of common peroneal entrapment neuropathy. Br Med J. 1969;56:623–626. PubMed
- Bahk MS, Cosgarea AJ. Physical examination and imaging of the lateral collateral ligament and posterolateral corner of the knee. Sports Med Arthrosc Rev. 2006;14:12–19. PubMed
- Orthopedic Physical Assessment by David J. Magee, 7th Edition.