Scapula Anatomy
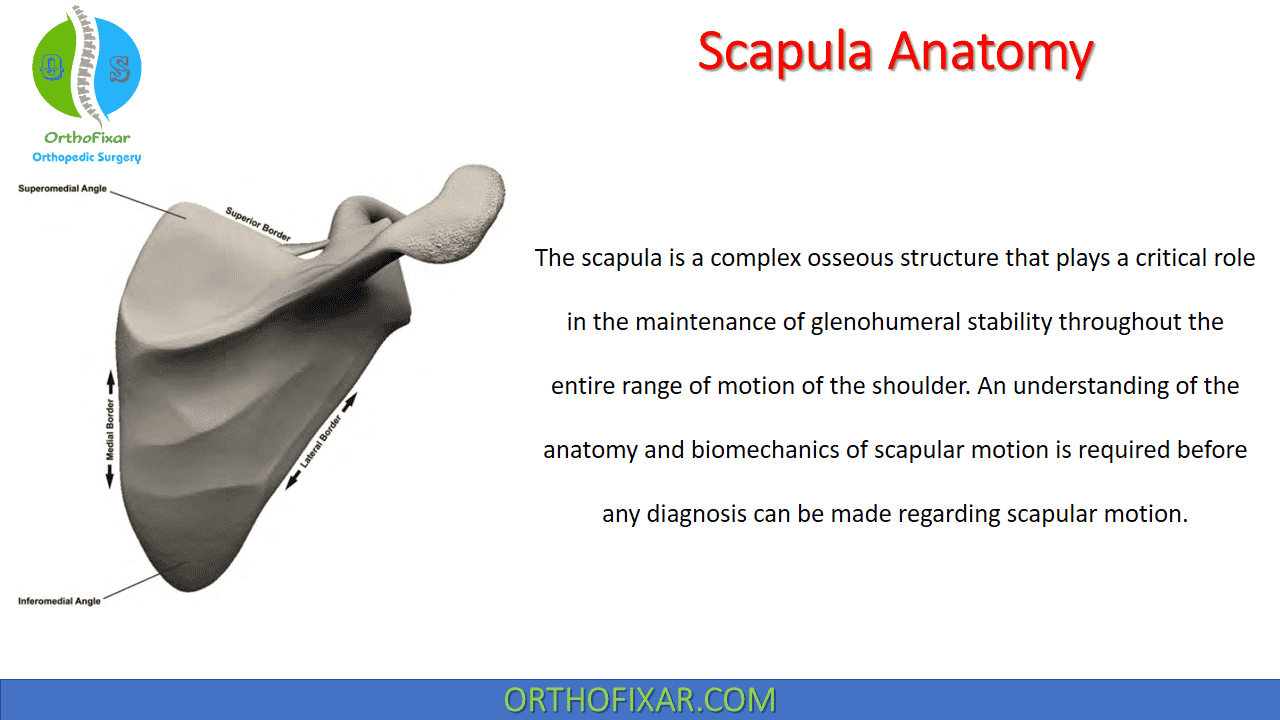
The Scapula Anatomy is a complex osseous structure that plays a critical role in the maintenance of glenohumeral stability throughout the entire range of motion of the shoulder. An understanding of the anatomy and biomechanics of scapular motion is required before any diagnosis can be made regarding scapular motion.
Scapula Anatomy & Biomechanics
The primary function of the scapula is to provide a stable fulcrum against which humeral elevation and rotation can occur. This is achieved through dynamic positioning of the glenoid to maximize glenohumeral contact through all planes of shoulder motion. A complete understanding of the osseous, muscular, bursal, and neurovascular anatomy along with the biomechanics of normal scapular motion is critical to the evaluation of any patient with shoulder pathology.
Therefore, an evaluation of scapular motion should be performed in each patient to prevent the development or progression of various shoulder conditions such as rotator cuff disease and glenohumeral instability.
Specific physical exam findings and observations related to scapular motion can have a significant effect on the approach to either operative or nonoperative management in patients who present with shoulder pain. As an example, increased upward rotation of the scapula may be a compensatory mechanism to prevent pain related to shoulder pathology whereas increased downward rotation may be factor associated with the production of shoulder pathology.
Osseous Anatomy
The scapula is a large, flat, triangular-shaped bone positioned over the posterior thorax between the second and seventh ribs. The scapula bone has three borders (superior, medial, and lateral) and two important angles (superomedial and inferomedial) that primarily serve as sites for muscles that attach to the scapula.
According to Lewitt, the three-dimensional resting position of the scapula is defined as being tilted anteriorly between 10° and 20° and medially rotated in the coronal plane between 30° and 40° (in other words, the glenoid faces more in the superior direction). The scapula is also angled anteriorly between 10° and 20° from the coronal plane. This position of anterior angulation is often referred to as the “scapular plane” when evaluating the shoulder.
While the general shape of the scapula bone is fairly consistent across the population, there exist several known topographical variations that may predispose some individuals to certain pathologic conditions (such as scapulothoracic bursitis or snapping scapula syndrome). For example, Aggarwal et al. performed measurements in 92 dried scapulae and found that the costal (anterior) surface of the scapula “undulated” and also varied in depth between 10.5 and 26.5 mm. The investigators noted that the thickness of the superomedial angle ranges between 2 and 4 mm whereas the inferomedial angle had a thickness between 5 and 8 mm. Anterior angulation of the superomedial angle also varied between 124° and 162° in the majority of their specimens.
In addition, the investigators also identified an anterior “horn-like” projection along the lateral border of at least one scapula. Several researchers have described other osseous abnormalities that may predispose some individuals to painful scapular snapping. These include the superomedial “bare area,” the “Luschka tubercle” (bony protuberance at the superomedial angle), the teres major tubercle (located at the insertion of this muscle), and anterior “hooking” of the superomedial angle.
The suprascapular notch is located near the junction of the lateral third of the superior scapular border, just medial to the confluence of the coracoid process with the scapular body. The anatomy of the suprascapular notch is also known to have various morphological features that may predispose some individuals to suprascapular nerve entrapment.
The transverse scapular ligament travels mediolaterally between the crests of the suprascapular notch. In most cases, the suprascapular nerve is found below the ligament and within the notch whereas the suprascapular artery is found above the ligament and outside of the notch. The transverse scapular ligament is also known to have significant anatomic variations that can also generate symptoms related to suprascapular nerve entrapment.

Scapula Muscles Anatomy
The scapulothoracic articulation is unique in that its motion is not dictated by osseous constraints. Rather, the scapula is positioned through the dynamic, coordinated action of surrounding periscapular muscles. Therefore, disruption or dysfunction of any one of these muscles can result in scapular malposition or dyskinetic motion which can lead to disordered shoulder function.
The intrinsic scapula muscles that attach to the scapula bone. These muscles are the four members of the rotator cuff and act to stabilize the glenohumeral joint. These include:
- Supraspinatus
- Infraspinatus
- Teres minor
- Subscapularis
See Also: Rotator Cuff of the Shoulder
The extrinsic scapula muscles attach to the processes of the scapula and affect motion at the glenohumeral joint. These include:
- Biceps brachii
- Triceps brachii
- Deltoid
- Trapezius
- Levator scapulae
- Serratus anterior
- Rhomboid major
- Rhomboid minor
- Latissmus dorsi
- Teres major
- Pectoralis minor
- Coracobrachialis
- Omohyoid
See Also: Scapular Dyskinesis

Scapula Bursae Anatomy
Bursae are fluid-filled sacs lined with synovial-like cells that facilitate gliding of opposing surfaces over one another. In the case of the scapula, there are several periscapular bursae that allow the scapula bone to glide smoothly over interposed muscle layers.
These scapula bursae are commonly defined as either “anatomic” or “adventitial” bursae, depending on their propensity to cause periscapular pain:
- Anatomic bursae are typically thought to represent normal, physiologic bursae that allow smooth gliding over the posterior thorax. The infraserratus and supraserratus bursae lie on either side of the serratus anterior muscle along the medial scapular border and are the most frequently recognized anatomic bursae.
- Adventitial bursae are most often located at the superomedial or inferomedial scapular angles and are thought to be significant pathological pain generators.
Some researchers have suggested that pain near the superomedial angle can be due to pathologic infraserratus or supraserratus bursal tissue, pain near the inferomedial angle is most likely the result of pathologic infraserratus bursal tissue, and pain near the confluence of the scapular spine may be caused by a pathologic scapulotrapezial bursa which is most commonly located deep to the trapezius and superficial to the scapular spine.


Neurovascular Scapula Anatomy
Knowledge of pertinent neurovascular scapula anatomy is necessary to fully evaluate any patient with a condition related to disordered shoulder motion. The spinal accessory nerve, which innervates the levator scapulae muscle, travels with the transverse cervical artery along the levator scapulae muscle which is situated deep to the trapezius muscle.
In some cases, the spinal accessory nerve may penetrate through the central portion of the levator scapulae. As the transverse cervical artery travels distally, it becomes the dorsal scapular artery which, in turn, travels with the dorsal scapular nerve beneath the rhomboid musculature a few fingerbreadths medial to the medial scapular border.
The long thoracic nerve is relatively protected as it travels along the anterior aspect of the serratus anterior muscle.
The suprascapular nerve arises from the superior trunk of the brachial plexus and courses towards the suprascapular notch with the suprascapular artery. As mentioned above, the suprascapular nerve passes beneath the transverse scapular ligament whereas the suprascapular artery travels above the ligament.

Scapula Biomechanics
With respect to normal shoulder kinematics, the scapula bone has several important functions that should be considered before evaluating any patient with a complaint related to the shoulder:
First, the scapula provides a stable fulcrum against which glenohumeral motion can occur through the dynamic action of the periscapular musculature, including the rotator cuff and deltoid muscles. External stabilization of the scapula may improve the contraction strength of the rotator cuff.
Second, accurate positioning of the scapula through coordinated muscle contractions facilitates glenohumeral articular congruency by maintaining alignment of opposing force couples, thus preserving the socalled concavity compression mechanism of dynamic stability.
Third, the scapula plays an important role in the transmission of force through the kinetic chain. In short, the scapula bone facilitates the transfer of kinetic and potential energy from the largest muscles of the core and trunk towards site of action. Dynamic scapular stability, which is facilitated by adequate core and trunk strength, is necessary to optimize the efficiency of this complex system. Perhaps one of the most well-known examples of this concept is the classic pitching motion most often utilized to deliver a high-velocity pitch in baseball.
References
- Aggarwal A, Wahee P, Harjeet, Aggarwal AK, Sahni D. Variable osseous anatomy of costal surface of scapula and its implications in relation to snapping scapula syndrome. Surg Radiol Anat. 2011 Mar;33(2):135-40. doi: 10.1007/s00276-010-0723-4. Epub 2010 Sep 1. PMID: 20809245.
- Cowan PT, Mudreac A, Varacallo M. Anatomy, Back, Scapula. [Updated 2021 Aug 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK531475/
- Boyle MJ, Misur P, youn SM, Ball CM. The superomedial bare area of the costal scapula surface: a possible cause of snapping scapula syndrome. Surg Radiol Anat. 2013;35(2):95–8.
- Milch H. Partial scapulectomy for snapping of the scapula. J Bone Joint Surg Am. 1950;32-A:561–6.
- Totlis T, Konstantinidis GA, Karanassos MT, Sofidis G, Anasasopoulos N, Natsis K. Bony structures related to snapping scapula: correlation to gender, side and age. Surg Radiol Anat. 2014;36(1):3–9.
- Edelson JG. Variations in the anatomy of the scapula with reference to the snapping scapula. Clin Orthop Relat Res. 1996;322:111–5.
- Millett PJ, Gaskill TR, Horan MP, van der Meijden O. Technique and outcomes of arthroscopic bursectomy and partial scapulectomy. Arthroscopy. 2012;28(12):1776–83.
- Polguj M, Jędrzejewski K, Podgórski M, Topol M. Correlation between morphometry of the suprascapular notch and anthropometric measurements of the scapula. Folia Morphol (Warsz). 2011;70(2):109–15.
- Polguj M, Jędrzejewski K, Podgórski M, Topol M. Morphometry study of the suprascapular notch: proposal of classification. Surg Radiol Anat. 2011;33(9): 781–7.
- Rockwood CA, Matsen FA. The shoulder. 2nd ed. Philadelphia, PA: WB Saunders Company; 2000.
- Wang JH, Chen C, Wu LP, Pan CQ, Zhang WJ, Li YK. Variable morphology of the suprascapular notch: an investigation and quantitative measurements in Chinese population. Clin Anat. 2011;24(1):47–55.
- Polguj M, Jędrzejewski K, Majos A, Topol M. Variations in bifi d superior transverse scapular ligament as a possible factor of suprascapular entrapment: an anatomical study. Int Orthop. 2012;36(10): 2095–100.
- Polguj M, Jędrzejewski K, Podgórski M, Majos A, Topol M. A proposal for classifi cation of the superior transverse scapular ligament: variable morphology and its potential influence on suprascapular nerve entrapment. J Shoulder Elbow Surg. 2013; 22(9):1265–73.
- Ciullo JV. Subscapular bursitis: treatment of “snapping scapula” or “wash-board” syndrome. Arthroscopy. 1992;8:412–3.
- Kuhne M, Boniquit N, Ghodadra N, Romeo AA, Provencher MT. The snapping scapula: diagnosis and treatment. Arthroscopy. 2009;25(11):1298–311.
- Cobey MC. The rolling scapula. Clin Orthop Relat Res. 1968;60:193–4.
- Percy EC, Birbrager D, Pitt MJ. Snapping scapula: a review of the literature and presentation of 14 patients. Can J Surg. 1988;31(4):248–50.
- Codman E. The shoulder. Malabar, FL: Krieger Publishing; 1984. p. 1–31.
- Kuhn JE, Plancher KD, Hawkins RJ. Symptomatic scapulothoracic crepitus and bursitis. J Am Acad Orthop Surg. 1998;6(5):267–73.
- Milch H. Snapping scapula. Clin Orthop. 1961;20:139–50.
- Sisto DJ, Jobe FW. The operative treatment of scapulothoracic bursitis in professional baseball pitchers. Am J Sports Med. 1986;14(3):192–4.
- Warth RJ, Spiegl UJ, Millett PJ. Scapulothoracic bursitis and snapping scapula syndrome: a critical review of current evidence. Am J Sports Med. 2015;43(1):236–45.
- Frank DK, Wenk E, Stern JC, Gottlieb RD, Moscatello AL. A cadaveric study of the motor nerves to the levator scapulae muscle. Otolaryngol Head Neck Surg. 1997;117:671–80.
- Ruland III LJ, Ruland CM, Matthews LS. Scapulothoracic anatomy for the arthroscopist. Arthroscopy. 1995;11(1):52–6.
- Kibler WB, Sciascia AD, Dome D. Evaluation of apparent and absolute supraspinatus strength in patients with shoulder injury using the scapular retraction test. Am J Sports Med. 2006;34(10):1643–7.
- Smith J, Dietrich CT, Kotajarvi BR, Kaufman KR. The effect of scapular protraction on isometric shoulder rotation strength in normal subjects. J Shoulder Elbow Surg. 2006;15(3):339–43.
- Merolla G, De Santis E, Campi F, Paladini P, Porcellini G. Supraspinatus and infraspinatus weakness in overhead athletes with scapular dyskinesis: strength assessment before and after restoration of scapular musculature balance. Musculoskelet Surg. 2010;94(3):119–25.
- Merolla G, De Santis E, Sperling JW, Campi F, Paladini P, Porcellini G. Infraspinatus strength assessment before and after scapular muscles rehabilitation in professional volleyball players with scapular dyskinesis. J Shoulder Elbow Surg. 2010;19(8):1256–64.
- Sciascia A, Thigpen C, Namdari S, Baldwin K. Kinetic chain abnormalities in the athletic shoulder. Sports Med Arthrosc. 2012;20(1):16–21.
- De May K, Danneels L, Cagnie B, Cools A. Are kinetic chain rowing exercises relevant in shoulder and trunk injury prevention training. Br J Sports Med. 2011;45(4):320.
May 16, 2023
OrthoFixar
Orthofixar does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice.
- Lifetime product updates
- Install on one device
- Lifetime product support
- Lifetime product updates
- Install on one device
- Lifetime product support
- Lifetime product updates
- Install on one device
- Lifetime product support
- Lifetime product updates
- Install on one device
- Lifetime product support