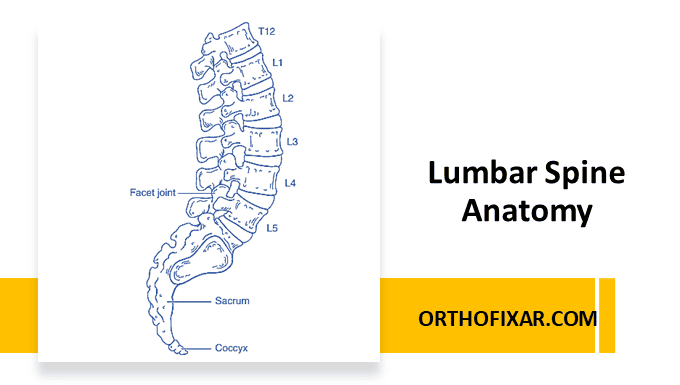
The lumbar spine consists of five vertebrae (L1–L5), each separated by an intervertebral disc that acts as a shock absorber. Its function is to support the body’s weight and allow a wide range of movement while protecting the spinal cord and nerve roots.
Below the fifth lumbar vertebra lies the sacrum, which connects the spine to the pelvis. Occasionally, variations such as lumbarization of S1 (a mobile sixth lumbar vertebra) or sacralization of L5 (fusion with the sacrum) may occur—these are called transitional vertebrae.
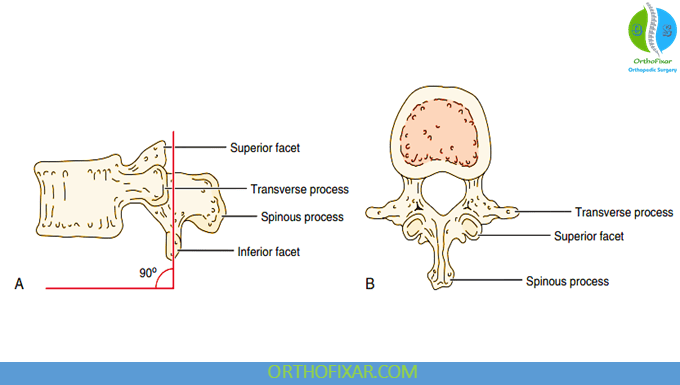
Lumbar Spine Facet Joints (Zygapophyseal)
There are 10 facet joints (five pairs) in the lumbar spine. These diarthrodial joints, also known as zygapophyseal or apophyseal joints, consist of a superior and an inferior articular facet covered by a fibrous capsule.
- Orientation:
- Superior facets face medially and backward and are typically concave.
- Inferior facets face laterally and forward and are convex.
- Function: Facet joints guide and limit motion. They allow flexion, extension, and side flexion, but rotation is minimal due to their orientation.
- Load Bearing: Normally, facet joints bear 20–25% of the axial load, but this can rise to 70% when intervertebral discs degenerate.
Facet tropism, a mismatch in facet orientation (common at L5–S1), can predispose to back pain and degeneration.
Close-packed position: Extension
Resting position: Midway between flexion and extension
Capsular pattern: Equal limitation of side flexion and rotation, followed by extension.
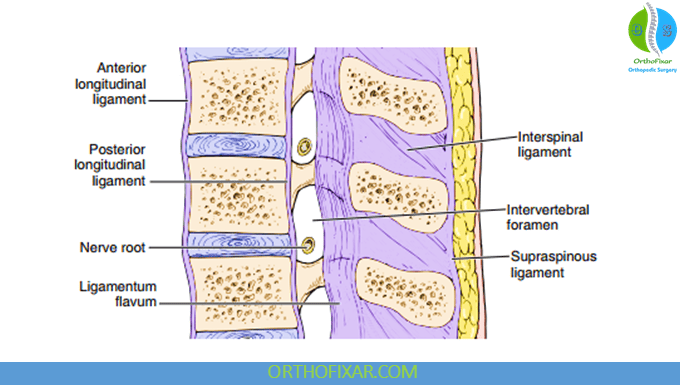
Ligaments of the Lumbar Spine
The lumbar spine is stabilized by several strong ligaments:
- Anterior and Posterior Longitudinal Ligaments
- Ligamentum Flavum
- Interspinous and Supraspinous Ligaments
- Intertransverse Ligaments
- Iliolumbar Ligament – unique to the lumbar region, connecting L5 transverse process to the posterior ilium. Its function is to prevent anterior displacement of L5 and enhances lumbopelvic stability.
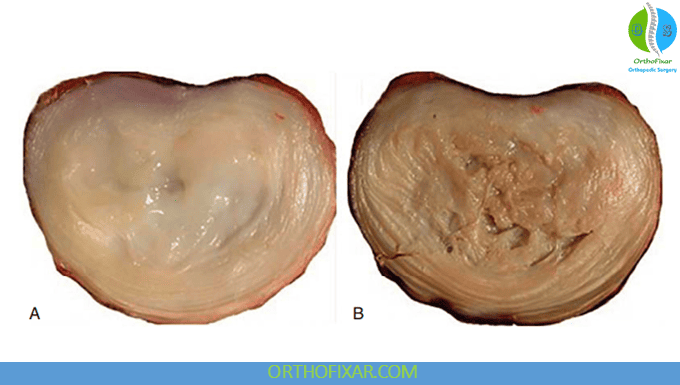
Intervertebral Discs
Intervertebral discs make up 20–25% of the total height of the vertebral column. Each disc has three components:
- Annulus Fibrosus – The tough outer ring made of 20 concentric collagen layers (Sharpey’s fibers) that resist torsion and shear.
- Nucleus Pulposus – The central, gelatinous core rich in mucopolysaccharides and water (≈85–90% at birth, ↓ to 65% with age). It provides shock absorption and allows movement between vertebrae.
- Cartilaginous End Plates – Thin layers (~1 mm) that anchor the disc to the vertebral body and permit nutrient diffusion, since discs are mostly avascular.
Disc Degeneration and Aging
With age, the disc loses water content and elasticity (a process known as spondylosis), reducing spinal height by 1–2 cm daily due to fluid shifts—a phenomenon known as diurnal variation.
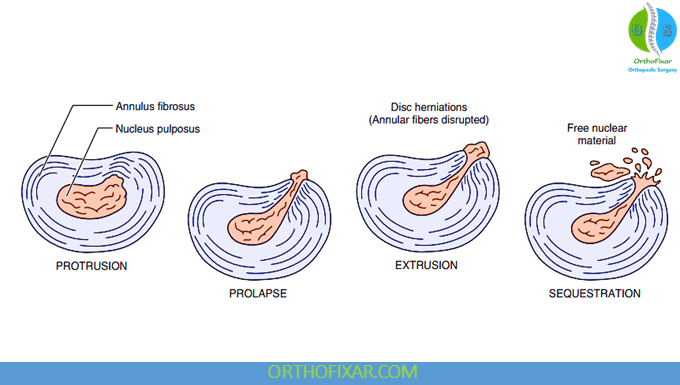
Common Disc Pathologies
Injury or degeneration of the intervertebral disc can lead to four main types of herniation:
- Protrusion – Disc bulge without rupture of the annulus fibrosus.
- Prolapse – Nucleus pulposus contained by only outermost fibers.
- Extrusion – Annulus is perforated; nucleus material enters the epidural space.
- Sequestration – Fragmented disc material migrates outside the disc.
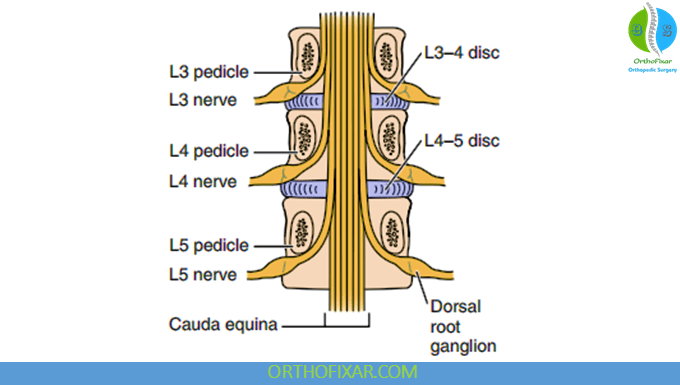
These conditions may compress:
- Spinal cord (upper lumbar) → myelopathy
- Cauda equina → saddle anesthesia, bladder/bowel dysfunction
- Nerve roots → radiculopathy (most common)
At the L4–L5 level, herniation typically compresses the L5 nerve root, not L4, due to root exit anatomy. The L5–S1 segment is the most common site of lumbar disc pathology, as it bears the greatest axial load and experiences high shearing stress.
See Also: Lumbar Plexus Anatomy
Biomechanics and Intradiscal Pressure
Posture significantly affects intradiscal pressure:
- Standing: Baseline pressure
- Forward flexion: Increases pressure
- Sitting slouched: Highest pressure
- Supine: Lowest pressure
Studies by Nachemson et al. revealed that posture and loading dramatically influence disc stress, highlighting the importance of ergonomics in preventing low back pain.
Nerve Supply and Pain Sources
The intervertebral disc itself is mostly aneural, but its outer annulus fibrosus receives limited innervation from:
- Sinuvertebral nerve
- Gray rami communicantes
Pain in the lumbar spine often arises from:
- Facet joint cartilage
- Longitudinal ligaments
- Nerve roots
- Vertebral body
See Also: Lumbar Spine Nerve Roots
See Also: S1 Nerve Root Examination
Clinical Relevance
Pathologic changes in the lumbar spine can lead to:
- Spondylosis – Degeneration of discs and vertebral bodies
- Spondylolysis – Pars interarticularis defect
- Spondylolisthesis – Forward vertebral slippage
- Retrolisthesis – Backward vertebral slippage
- Facet joint arthropathy – Painful degeneration of the posterior elements
Summary
| Structure | Function | Clinical Note |
|---|---|---|
| Facet Joints | Guide motion, bear load | Source of mechanical low back pain |
| Intervertebral Disc | Shock absorption, motion | Common site of herniation |
| Iliolumbar Ligament | Stabilizes L5–S1 | Prevents anterior shear |
| End Plate | Nutrient diffusion | Site of Schmorl’s nodes |
| L5–S1 Level | Transition between mobile & fixed segments | Highest stress, common degeneration site |
Key Takeaways
- Lumbar spine consists of five vertebrae, five pairs of facet joints, and intervertebral discs that distribute load and permit motion.
- Facet joints guide movement; discs absorb shock.
- L5–S1 is the most stress-prone segment.
- Degenerative and herniation processes are the most common causes of low back pain.
References & More
- Frymoyer JW, Akeson W, Brandt K, et al. Clinical perspectives. In: Frymoyer JW, Gordon SL, eds. New Perspectives in Low Back Pain. Park Ridge, IL: American Academy of Orthopedic Surgeons; 1989.
- Beattie P. Current understanding of lumbar intervertebral disc degeneration: a review with emphasis upon etiology, pathophysiology, and lumbar magnetic resonance imaging findings. J Orthop Sports Phys Ther. 2008;38:329–340. PubMed
- Taylor JR, Twomey LT. Structure and function of lumbar zygapophyseal (facet) joints. In: Boyling JD, Palastanga N, eds. Grieve’s Modern Manual Therapy: The Vertebral Column. 2nd ed. Edinburgh: Churchill Livingstone; 1994.
- Fujiwana A, Tamai K, Yoshida H, et al. Anatomy of the iliolumbar ligament. Clin Orthop Relat Res. 2000;380:167–172 PubMed
- Aihara T, Takahashi K, Yamagata M, et al. Does the iliolumbar ligament prevent anterior displacement of the fifth lumbar vertebra with defects of the pars? J Bone Joint Surg Br. 2000;82:846–850. PubMed
- Roughley PJ. Biology of intervertebral disc aging and degeneration – involvement of the extra cellular matrix. Spine. 2004;29(23):2691–2699. PubMed
- Coventry MB, Ghormley RK, Kernohan JW. The intervertebral disc: its microscopic anatomy and pathology. Part I: Anatomy, development and physiology; Part II: Changes in the intervertebral disc concomitant with age; Part III: Pathological changes in the intervertebral disc. J Bone Joint Surg. 1945;27:105 (Part I), 233 (Part II), 460 (Part III).
- Rodriquez AG, Slichter CK, Acosta FL, et al. Human disc nucleus properties and vertebral endplate permeability. Spine. 2011;36(7):512–520. PubMed
- Bogduk N. The innervation of the lumbar spine. Spine. 1983;8:286–293. PubMed
- Borenstein DG, Wiesel SW, Boden SD: Low back pain: medical diagnosis and comprehensive management, Philadelphia, 1995, WB Saunders.
- Vo NV, Hartman RA, Patil PR, et al: Molecular mechanisms of biological aging in intervertebral discs, J Orthop Res 34:1292, 2016. Courtesy Dr. Ian Stokes.
- Orthopedic Physical Assessment by David J. Magee, 7th Edition.
Closed.