Assessment of the popliteal artery pulse is a fundamental component of the lower limb vascular examination. Although more challenging to palpate than other peripheral pulses, accurate technique and anatomical knowledge improve detection and clinical interpretation.
This guide explains the exact location, step-by-step palpation technique, and clinical significance of the popliteal pulse, based on standard physical examination references and vascular medicine principles.
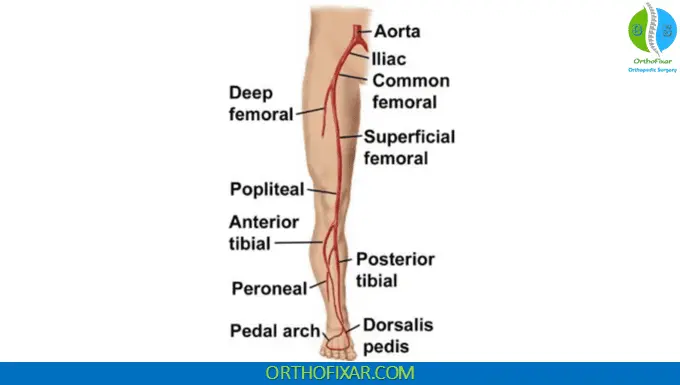
Anatomy of the Popliteal Artery
The Popliteal artery is the continuation of the Femoral artery after it passes through the adductor hiatus. It travels deep within the popliteal fossa, posterior to the knee joint, before dividing into the anterior and posterior tibial arteries.
Key anatomical points:
- Located deep in the popliteal fossa
- Lies against the posterior surface of the femur
- Covered by fat and connective tissue
- More difficult to palpate than superficial pulses (e.g., dorsalis pedis)
Because of its depth and surrounding structures, the popliteal pulse typically feels diffuse and less distinct.
See Also: Femoral Artery Pulse Location & Palpation
Popliteal Pulse Location
The popliteal pulse is palpated:
- Behind the knee
- In the midline of the popliteal fossa
- With the knee slightly flexed
- Using deep pressure
Due to its depth, firm and deliberate palpation is required.
Step-by-Step: How to Palpate the Popliteal Pulse (Supine Position)
This is the standard examination method recommended in clinical physical diagnosis texts.
Patient Position:
- The patient lies supine
- The knee is somewhat flexed
- The leg must be fully relaxed
Examiner Technique:
- Support the patient’s leg with both hands.
- Place the fingertips of both hands so they meet at the midline behind the knee.
- Press deeply into the popliteal fossa.
- Maintain steady pressure and feel for pulsation.
Important Clinical Note:
- The popliteal pulse is deeper and more diffuse than other peripheral pulses.
- It may be difficult to detect even in healthy individuals.

Alternative Method: Prone Position Technique
If the pulse cannot be palpated using the supine method, try the prone approach.
Patient Position:
- Patient lies prone
- Knee flexed to approximately 90°
- Lower leg relaxed against the examiner’s shoulder or upper arm
Examiner Technique:
- Press both thumbs deeply into the popliteal fossa
- Apply firm, sustained pressure
This method sometimes allows better localization due to improved muscle relaxation.

Why is the Popliteal Pulse Difficult to Find?
Several anatomical and clinical factors contribute:
- The artery is deeply positioned
- Surrounded by adipose tissue
- Lies close to bone
- May be obscured in obese or muscular patients
Failure to palpate does not automatically indicate pathology; correlation with other pulses is essential.
Clinical Significance of the Popliteal Pulse
1. Peripheral Arterial Disease (PAD)
Atherosclerosis most commonly obstructs arteries in the thigh region. Typical findings include:
- Normal femoral pulse
- Decreased or absent popliteal pulse
This pattern strongly suggests arterial obstruction between the femoral and popliteal levels. Peripheral arterial disease is most commonly caused by atherosclerosis and increases with age.
2. Popliteal Artery Aneurysm
An exaggerated, widened popliteal pulse suggests a popliteal artery aneurysm. A Popliteal artery aneurysm is:
- An abnormal dilation of the popliteal artery
- Usually caused by atherosclerosis
- More common in men ≥50 years
- Often associated with femoral aneurysms
Although popliteal and femoral aneurysms are uncommon, they are clinically significant because they can cause:
- Thrombosis
- Embolization
- Acute limb ischemia
Early detection through careful palpation is critical.
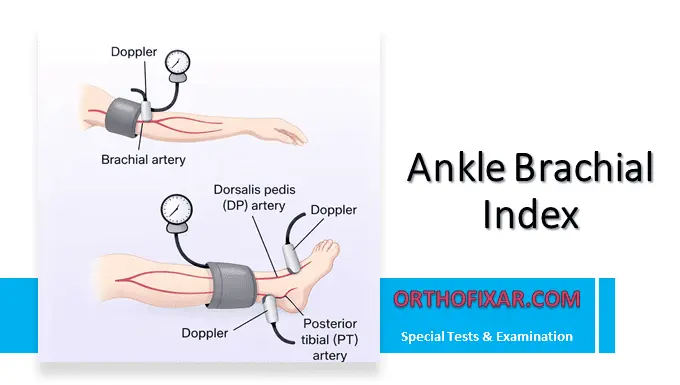
Comparison with Other Lower Limb Pulses
During a complete vascular exam, always assess:
- Femoral artery pulse
- Dorsalis pedis pulse
- Posterior tibial pulse
A systematic approach allows identification of the level of arterial obstruction.
Example pattern:
- Femoral pulse present
- Popliteal pulse absent: Suggests superficial femoral artery disease
Key Clinical Pearls
- Always ensure the leg is relaxed
- Use deep, steady pressure
- Compare bilaterally
- If not palpable supine, try the prone 90° flexion method
- A widened pulse warrants evaluation for aneurysm
- A decreased pulse with normal femoral pulse suggests atherosclerotic obstruction
FAQ
Why is the popliteal pulse harder to feel than other pulses?
The popliteal artery lies deep in the popliteal fossa and feels more diffuse than superficial pulses like the dorsalis pedis
What does an absent popliteal pulse indicate?
It may suggest:
– Peripheral arterial disease
– Thigh-level atherosclerotic obstruction
However, improper technique must first be excluded.
What does a bounding popliteal pulse mean?
An exaggerated or widened pulse may indicate a popliteal artery aneurysm, especially in men over 50 with vascular risk factors.
Should both legs always be examined?
Yes. Always compare both sides to detect asymmetry.
References & More
- Popliteal artery – Wikipedia
- Myers KA, Scott DF, Devine TJ, Johnston AH, Denton MJ, Gilfillan IS. Palpation of the femoral and popliteal pulses: a study of the accuracy as assessed by agreement between multiple observers. Eur J Vasc Surg. 1987 Aug;1(4):245-9. doi: 10.1016/s0950-821x(87)80075-0. PMID: 3454755. Pubmed
- Zimmerman B, Williams D. Peripheral Pulse. [Updated 2025 Jul 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: Pubmed
- Ger R. Palpation of the popliteal pulse. Surgery. 1966 Sep;60(3):615-6. PMID: 5913788.
- Bickley, L. S., Szilagyi, P. G., Hoffman, R. M., & Soriano, R. P. (2021). Bates’ guide to physical examination and history taking, 12e.