The femoral artery pulse is one of the most important peripheral pulses assessed during a physical examination. Accurate palpation of the femoral pulse provides valuable diagnostic information about lower limb perfusion, central circulation, and potential vascular pathology such as peripheral arterial disease (PAD) or femoral artery aneurysm.
In this article, we will explain the anatomical location of the femoral pulse, the correct palpation technique, and the clinical significance of abnormal findings—based on standard clinical examination references and trusted medical sources.
Anatomy of the Femoral Artery
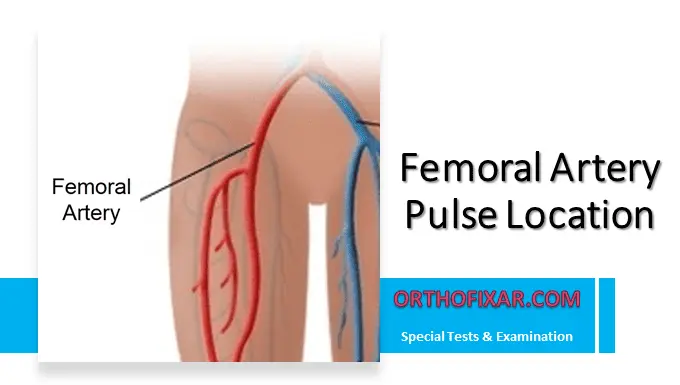
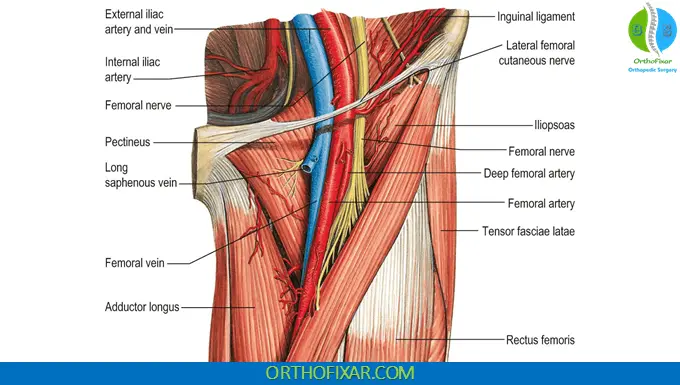
The femoral artery is a continuation of the external iliac artery. It begins as the vessel passes beneath the inguinal ligament and enters the femoral triangle of the upper thigh.
Key Anatomical Landmarks
To locate the femoral pulse:
- Identify the inguinal ligament
- Find the anterior superior iliac spine (ASIS)
- Locate the symphysis pubis
The femoral artery runs below the inguinal ligament, approximately midway between the anterior superior iliac spine and the symphysis pubis.
A helpful anatomical mnemonic within the femoral triangle is NAVL (lateral to medial):
- Nerve
- Artery
- Vein
- Lymphatics
The femoral artery lies medial to the femoral nerve and lateral to the femoral vein.
How to Palpate the Femoral Artery Pulse?
Step-by-Step Technique
- Position the patient supine with hips slightly abducted and externally rotated.
- Locate the midpoint between:
- The anterior superior iliac spine
- The symphysis pubis
- Place your fingers just below the inguinal ligament.
- Press deeply to palpate the pulse.
Because the femoral artery is located deep within the soft tissue, firm pressure is required.
See Also: Radial Pulse Location
Tip for Obese Patients
As in deep abdominal palpation, using two hands (one placed over the other) can improve detection of the pulse, especially in obese patients. Avoid using your thumb, as it may transmit your own pulse.

Clinical Significance of the Femoral Pulse
1. Absent Femoral Pulse and Peripheral Arterial Disease (PAD)
An absent femoral pulse is a highly significant finding.
- The Likelihood Ratio (LR) of PAD is greater than 6.26 when the femoral pulse is absent.
- This strongly increases the probability of peripheral arterial disease.
Peripheral arterial disease is commonly caused by atherosclerosis and leads to reduced blood flow to the lower extremities.
If the occlusion is located at the aortic or iliac level, all pulses distal to the blockage (popliteal, posterior tibial, dorsalis pedis) are typically diminished or absent.
You may also observe:
- Postural color changes
- Pallor on elevation
- Dependent rubor
See Also: Ankle Brachial Index (ABI)
2. Exaggerated or Bounding Femoral Pulse
An exaggerated, widened femoral pulse may suggest:
Aneurysmal dilation can present as:
- A pulsatile mass in the groin
- Expansile pulsation
- Bruit on auscultation
This condition requires further vascular imaging such as duplex ultrasonography.
3. Bilateral Comparison is Essential
Always compare both sides:
- Symmetry suggests normal perfusion.
- Asymmetry may indicate unilateral arterial obstruction.
- Bilateral absence raises suspicion for proximal (aortic or iliac) occlusion.
Common Clinical Errors to Avoid
- Palpating too medially (you may feel the femoral vein instead)
- Not applying enough pressure
- Failing to compare both sides
- Confusing transmitted abdominal aortic pulsations with femoral pulsation
When Should You Check the Femoral Pulse?
Femoral pulse palpation is particularly important in:
- Suspected peripheral arterial disease
- Acute limb ischemia
- Shock assessment
- Trauma evaluation
- Cardiovascular examination
- Pre- and post-catheterization monitoring
Clinical Summary
The femoral artery pulse is palpated:
- Below the inguinal ligament
- Midway between the anterior superior iliac spine and the symphysis pubis
- Using firm, deep pressure
Key Clinical Points
- Absent pulse → Strongly suggests PAD (LR > 6.26)
- All distal pulses absent → Consider aortic or iliac occlusion
- Bounding pulse → Consider femoral aneurysm
- Always compare bilaterally
Final Thoughts
Accurate assessment of the femoral artery pulse is a fundamental component of the vascular physical examination. Mastering proper landmark identification and palpation technique allows early detection of serious vascular conditions such as peripheral arterial disease and femoral artery aneurysm.
FAQ
Where exactly is the femoral artery pulse located?
The pulse of the femoral artery is palpated just below the inguinal ligament, approximately midway between the anterior superior iliac spine (ASIS) and the symphysis pubis.
It lies within the femoral triangle and is positioned:
– Medial to the femoral nerve
– Lateral to the femoral vein
– Firm, deep pressure is required because the artery lies beneath soft tissue.
Why is the femoral pulse important in clinical examination?
The femoral pulse is a key component of the vascular assessment of the lower limb. It helps evaluate:
– Arterial perfusion
– Presence of proximal arterial occlusion
– Cardiovascular stability in trauma or shock
– Suspected Peripheral Arterial Disease
Its presence confirms blood flow from the aorta and iliac arteries to the lower extremity.
What does an absent femoral pulse indicate?
An absent femoral pulse significantly increases the probability of peripheral arterial disease (PAD).
– The Likelihood Ratio (LR) is > 6.26, which strongly supports the diagnosis.
– If the occlusion is at the aortic or iliac level, all pulses distal to the obstruction (popliteal, posterior tibial, dorsalis pedis) are usually absent.
Bilateral absence may suggest proximal large-vessel disease.
What does a bounding or exaggerated femoral pulse suggest?
A widened or bounding femoral pulse may indicate:
– Arterial dilation
– Possible femoral artery aneurysm
A femoral aneurysm may present as:
– A pulsatile groin mass
– Expansile pulsation
– Possible bruit on auscultation
Further evaluation with duplex ultrasonography is recommended.
How do you palpate the femoral pulse correctly?
To palpate effectively:
– Position the patient supine.
– Identify the midpoint between the ASIS and symphysis pubis.
– Place your fingers below the inguinal ligament.
– Apply deep, steady pressure.
In obese patients, placing one hand over the other may improve detection.
Avoid using your thumb to prevent mistaking your own pulse for the patient’s.
Can the femoral pulse be used during emergencies?
Yes. The femoral pulse is often assessed in:
– Trauma settings
– Cardiac arrest situations
– Severe hypotension
– Advanced life support scenarios
Because it is a central pulse, it may still be palpable when distal pulses are absent.
What is the difference between femoral and popliteal pulses?
The femoral pulse is located in the groin and reflects proximal arterial flow, while the popliteal pulse is located behind the knee and assesses more distal circulation.
If the femoral pulse is present but the popliteal pulse is absent, the obstruction is likely between those two anatomical levels.
Why might the femoral pulse be difficult to feel?
Common reasons include:
– Obesity
– Excess soft tissue
– Incorrect landmark identification
– Insufficient pressure
– Severe hypotension
– Arterial occlusion
Using proper anatomical landmarks and adequate depth of palpation improves accuracy.
References & More
- Zimmerman B, Williams D. Peripheral Pulse. [Updated 2025 Jul 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: Pubmed
- Bickley, L. S., Szilagyi, P. G., Hoffman, R. M., & Soriano, R. P. (2021). Bates’ guide to physical examination and history taking, 12e.
- Khammari Nystrom F, Petersson G, Stephansson O, Johansson S, Altman M. Diagnostic values of the femoral pulse palpation test. Arch Dis Child Fetal Neonatal Ed. 2020 Jul;105(4):375-379. doi: 10.1136/archdischild-2019-317066. Epub 2019 Oct 9. PMID: 31597727. Pubmed