Core body temperature reflects the temperature of the body’s internal environment and is a vital indicator of physiologic function. Accurate temperature assessment is fundamental in clinical practice, as deviations may signal infection, metabolic disorders, environmental exposure, or systemic disease.
What Is Core Body Temperature?
Core body temperature is the temperature of deep tissues such as the brain, thoracic organs, and abdominal organs. In healthy adults, the average core body temperature is approximately 37°C (98.6°F).
However, this value is not fixed. Core temperature normally:
- Fluctuates by about 1°C (1.8°F) throughout the day
- Is lowest in the early morning
- Peaks in the afternoon and early evening
Women generally exhibit a wider normal temperature range than men, partly due to hormonal variations during the menstrual cycle.
Gold Standard vs Clinical Measurement
The research gold standard for measuring core body temperature is blood temperature in the pulmonary artery. While highly accurate, this method is invasive and impractical for routine care.
In everyday clinical practice, noninvasive methods are used instead, including:
- Oral
- Rectal
- Axillary
- Tympanic membrane
- Temporal artery
Tympanic membrane and temporal artery methods use infrared thermometry.
See Also: Blood Pressure Measurement

Comparison of Temperature Measurement Sites
Oral Temperature
- Common and convenient
- Typically lower than true core temperature
- On average:
- 0.4–0.5°C (0.7–0.9°F) lower than rectal
- About 1°C higher than axillary
- Influenced by:
- Hot or cold beverages
- Smoking
- Rapid breathing
Technique (Electronic thermometer):
- Place disposable probe cover
- Insert under the tongue
- Ask the patient to close lips
- Wait ~10 seconds for reading
Important: Delay measurement 10–15 minutes after eating, drinking, or smoking.
Rectal Temperature
- Most accurate noninvasive estimate of core temperature
- Preferred in:
- Infants
- Critically ill patients
- Situations with rapid breathing
Technique:
- Position patient on side with hip flexed
- Lubricate thermometer
- Insert 3–4 cm (1.5 inches) toward the umbilicus
- Wait:
- 3 minutes (glass)
- ~10 seconds (electronic)
Axillary Temperature
- Least accurate method
- Takes 5–10 minutes to register
- Often underestimates core temperature
- Used mainly when other methods are not feasible
Tympanic Membrane Temperature
The tympanic membrane shares blood supply with the hypothalamus, the brain’s temperature-regulating center.
Advantages:
- Rapid (2–3 seconds)
- Noninvasive
Limitations:
- More variable than oral or rectal
- Accuracy depends on:
- Proper probe positioning
- Absence of cerumen (earwax)
Studies suggest tympanic temperatures are about 0.5°C lower than pulmonary artery temperature.
Temporal Artery Temperature
This method measures infrared heat over the temporal artery, which runs close to the skin surface.
Technique:
- Place probe on the center of the forehead
- Press scan button
- Sweep across forehead, down the cheek, and behind the ear
- Read the highest recorded temperature
Evidence suggests that combined forehead and behind-the-ear scanning is more accurate than forehead scanning alone.
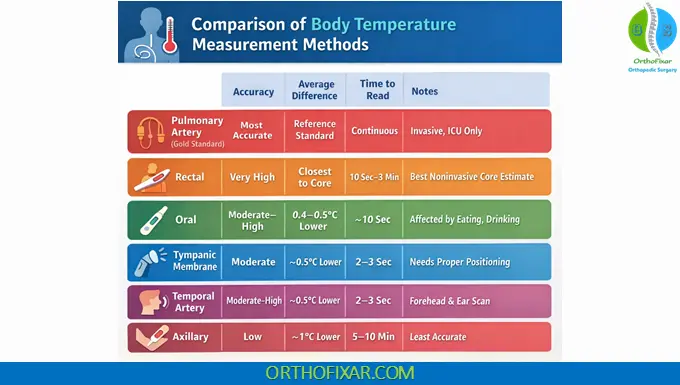
Comparison of Core Body Temperature Measurement Methods
| Measurement Method | Typical Accuracy vs Core Temp | Average Difference | Time to Read | Advantages | Limitations / Notes |
|---|---|---|---|---|---|
| Pulmonary Artery (Gold Standard) | Most accurate | Reference standard | Continuous | Direct measurement of core temperature | Invasive, ICU-only, not used routinely |
| Rectal | Very high | Closest to core | 10 sec–3 min | Best noninvasive estimate of core temperature; reliable in infants and critically ill patients | Invasive, patient discomfort, contraindicated in neutropenia or rectal pathology |
| Oral | Moderate–high | ~0.4–0.5°C lower than rectal | ~10 sec | Easy, widely used, inexpensive | Affected by hot/cold drinks, smoking, rapid breathing |
| Tympanic Membrane | Moderate | ~0.5°C lower than core | 2–3 sec | Fast, noninvasive, reflects hypothalamic blood supply | Technique-sensitive; cerumen reduces accuracy |
| Temporal Artery | Moderate–high | ~0.5°C lower than core | 2–3 sec | Quick, well tolerated, good for screening | Accuracy depends on proper scanning technique |
| Axillary | Low | ~1°C lower than oral | 5–10 min | Safe, noninvasive, useful when other sites unavailable | Least accurate; slow response time |
Fever, Hyperpyrexia, and Hypothermia
Fever (Pyrexia)
An elevation of body temperature above normal.
Common causes include:
- Infection
- Trauma (surgery, crush injuries)
- Malignancy
- Drug reactions
- Immune-mediated diseases (e.g., collagen vascular disorders)
Hyperpyrexia
- Extreme elevation of temperature
- Defined as >41.1°C (106°F)
- Medical emergency requiring urgent evaluation
Hypothermia
- Abnormally low body temperature
- Defined as <35°C (95°F) rectally
Causes include:
- Cold exposure (most common)
- Reduced movement (e.g., paralysis)
- Impaired vasoconstriction (sepsis, alcohol)
- Starvation
- Hypothyroidism
- Hypoglycemia
Older adults are particularly vulnerable and may:
- Develop hypothermia more easily
- Fail to mount a fever response during infection
Clinical Considerations
- Rapid respiratory rates increase the discrepancy between oral and rectal temperatures
- In such cases, rectal measurements are more reliable
- Always interpret temperature values in clinical context, not in isolation
Key Takeaway
Core body temperature is a dynamic vital sign influenced by time of day, measurement method, patient characteristics, and clinical condition. Understanding the strengths and limitations of each measurement technique ensures accurate assessment and appropriate clinical decision-making.
References & More
- Hymczak H, Gołąb A, Mendrala K, Plicner D, Darocha T, Podsiadło P, Hudziak D, Gocoł R, Kosiński S. Core Temperature Measurement-Principles of Correct Measurement, Problems, and Complications. Int J Environ Res Public Health. 2021 Oct 10;18(20):10606. doi: 10.3390/ijerph182010606. PMID: 34682351; PMCID: PMC8535559. Pubmed
- Janke D, Kagelmann N, Storm C, Maggioni MA, Kienast C, Gunga HC, Opatz O. Measuring Core Body Temperature Using a Non-invasive, Disposable Double-Sensor During Targeted Temperature Management in Post-cardiac Arrest Patients. Front Med (Lausanne). 2021 May 5;8:666908. doi: 10.3389/fmed.2021.666908. PMID: 34026794; PMCID: PMC8132874. Pubmed
- Bickley, L. S., Szilagyi, P. G., Hoffman, R. M., & Soriano, R. P. (2021). Bates’ guide to physical examination and history taking, 12e.