Pain assessment is a core clinical skill and one of the most common reasons patients seek medical care. Understanding the difference between acute pain and chronic pain, and assessing each correctly, is essential for safe treatment, improved function, and patient trust.
This guide explains how to assess pain systematically, using evidence-based tools and a multidisciplinary approach.
What Is Pain?
According to the International Association for the Study of Pain (IASP), pain is:
“An unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage.”
Pain is not only physical. It involves:
- Sensory perception
- Emotional response
- Cognitive interpretation
Pain can exist even when imaging and laboratory tests are normal. This is a medical reality, not a diagnostic failure.
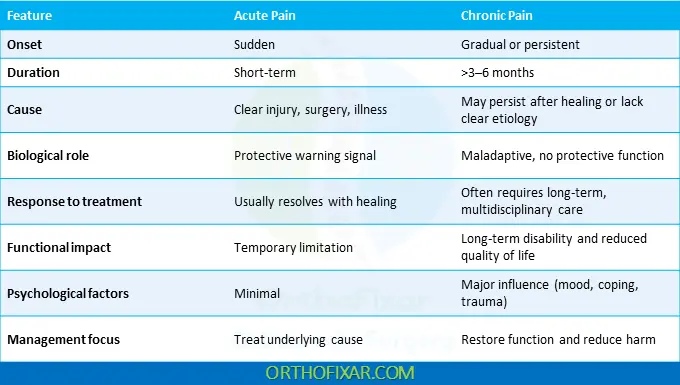
Acute Pain vs Chronic Pain
Acute Pain
Acute pain features include:
- It occurs suddenly
- It’s usually linked to injury, surgery, or illness
- It has a protective biological function
- It resolves as healing occurs
Chronic Pain
Chronic pain is defined as:
- Pain lasting more than 3–6 months
- Pain persisting beyond normal tissue healing
- Pain that recurs over months or years
Chronic non-cancer pain:
- Affects ~100 million Americans
- Accounts for 5%–33% of primary care visits
- Is the leading cause of long-term disability
Over 40% of patients report inadequate pain control, highlighting the need for better assessment and follow-up.
Why Accurate Pain Assessment Matters
Pain is multifactorial. It is influenced by:
- Tissue damage
- Nervous system changes
- Mental health
- Social and cultural factors
- Prior trauma
A measurement-based, patient-centered approach improves outcomes and reduces unsafe medication use.
Listening to the patient’s pain story is not optional—it is diagnostic.
How to Take a Complete Pain History
1. Onset and Pattern
Ask:
- When did the pain start?
- Was it related to injury or illness?
- Is it constant or intermittent?
- Does it change with time of day or movement?
2. Pain Characteristics
Assess:
- Location (ask the patient to point)
- Quality (sharp, dull, burning, electric)
- Radiation or pattern
- Aggravating and relieving factors
3. Previous Treatments
Review:
- Medications (past and current)
- Physical therapy
- Injections or procedures
- Complementary therapies
A thorough medication history prevents dangerous interactions.
4. Comorbid Conditions
Conditions that strongly affect pain perception include:
- Arthritis
- Diabetes
- HIV/AIDS
- Sickle cell disease
- Depression and anxiety
- Substance use disorders
Ignoring comorbidities leads to treatment failure.
5. Functional Impact
Ask how pain affects:
- Daily activities
- Sleep quality
- Mood and concentration
- Work and productivity
- Sexual activity
Pain that limits function is clinically significant—regardless of imaging results.
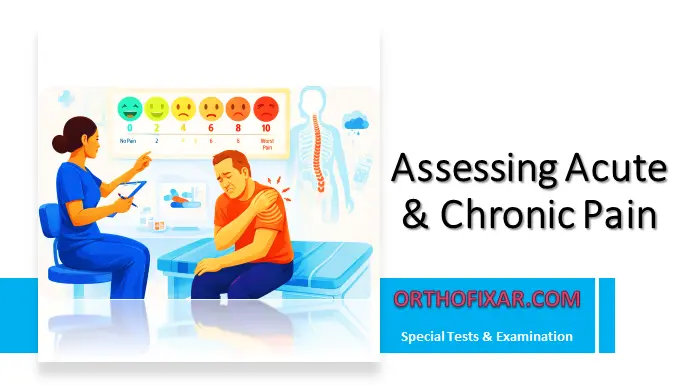
Assessing Pain Severity: Standard Pain Scales
Consistent measurement is essential.
Common Pain Severity Scales
- Numeric Rating Scale (0–10)
- Visual Analog Scale (VAS)
- Wong-Baker FACES Pain Rating Scale
The Wong-Baker FACES® scale is especially useful for:
- Children
- Patients with language barriers
- Cognitive impairment
Multidimensional Pain Tools
- Brief Pain Inventory
- McGill Pain Questionnaire
These tools assess both pain intensity and its impact on daily life.
See Also: LANSS Pain Scale
Health Disparities in Pain Assessment
Research shows clear disparities in pain treatment:
- Lower use of analgesics in minority populations
- Unequal management of cancer, postoperative, and low back pain
Contributing factors include:
- Implicit clinician bias
- Language barriers
- Communication failures
Standardized pain assessment tools reduce bias and improve equity in care.
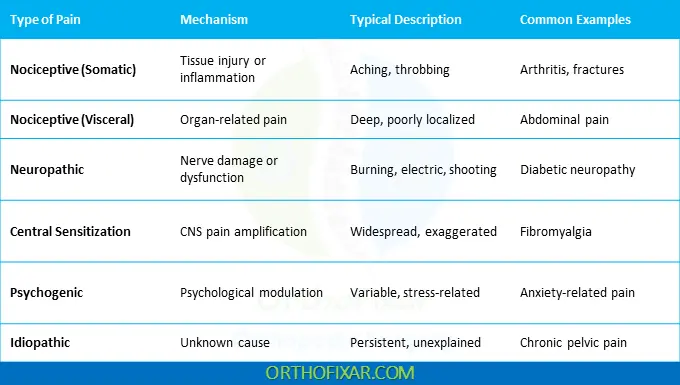
Types of Pain
Nociceptive Pain
- Caused by tissue injury or inflammation
- Nervous system intact
- Examples: arthritis, spinal stenosis
- Can be acute or chronic
Neuropathic Pain
- Caused by nerve injury or disease
- Burning, shooting, or electric pain
- May persist after healing
Central Sensitization Pain
- Amplified pain processing in the central nervous system
- Lower pain threshold
- Example: fibromyalgia
Psychogenic Pain
- Strongly influenced by mental health, coping style, and social factors
Idiopathic Pain
- Pain without identifiable cause
- Still real and clinically relevant
Managing Chronic Pain: Measurement-Based Care
Chronic pain management requires structured monitoring.
Key Steps in Chronic Pain Assessment
- Measure pain intensity and interference with daily life
- Screen for depression, anxiety, and PTSD
- Evaluate sleep quality
- Assess risk of substance use disorders
- Monitor opioid dose and equivalents
This approach improves safety and treatment precision.
Opioids and Chronic Pain: A Cautionary Note
Opioid prescriptions have increased dramatically over recent decades. While opioids have a role in selected cases, risks rise sharply with:
- High daily doses
- Older age
- Depression or substance use
- Concurrent benzodiazepines
Effective pain management prioritizes:
- Non-opioid therapies
- Physical rehabilitation
- Behavioral interventions
- Careful monitoring
Poor pain assessment directly leads to poor—and sometimes fatal—treatment decisions.
Key Takeaways
- Pain assessment must be systematic and patient-centered
- Chronic and Acute pain require different clinical strategies
- Functional impact matters as much as pain intensity
- Measurement-based care improves outcomes and safety
Pain is real—even when tests are normal. Assess it seriously, or expect treatment failure.
References & More
- Chou R, Wagner J, Ahmed AY, et al. Treatments for Acute Pain: A Systematic Review [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2020 Dec. (Comparative Effectiveness Review, No. 240.) Introduction. Available from: Pubmed
- National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Health Care Services; Committee on Evidence-Based Clinical Practice Guidelines for Prescribing Opioids for Acute Pain. Framing Opioid Prescribing Guidelines for Acute Pain: Developing the Evidence. Washington (DC): National Academies Press (US); 2019 Dec 19. 2, Managing Acute Pain. Available from: Pubmed
- Carr DB, Goudas LC. Acute pain. Lancet. 1999 Jun 12;353(9169):2051-8. doi: 10.1016/S0140-6736(99)03313-9. PMID: 10376632. Pubmed
- Bickley, L. S., Szilagyi, P. G., Hoffman, R. M., & Soriano, R. P. (2021). Bates’ guide to physical examination and history taking, 12e.