The sural nerve represents one of the most clinically significant sensory nerves in the lower extremity, serving as both a crucial component of peripheral sensation and a valuable resource for nerve grafting procedures. Understanding its detailed anatomy is essential for medical professionals involved in orthopedic surgery, neurology, plastic surgery, and podiatry.
Embryological Development and Formation
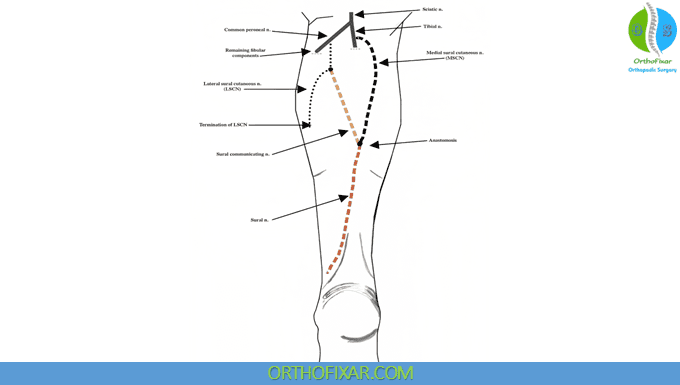
The sural nerve develops from the fusion of two distinct neural components during embryogenesis. The medial sural cutaneous nerve arises from the tibial nerve, while the lateral sural cutaneous nerve originates from the common fibular nerve. This dual origin explains the anatomical variations frequently encountered in clinical practice and underscores the importance of understanding the nerve’s developmental biology.
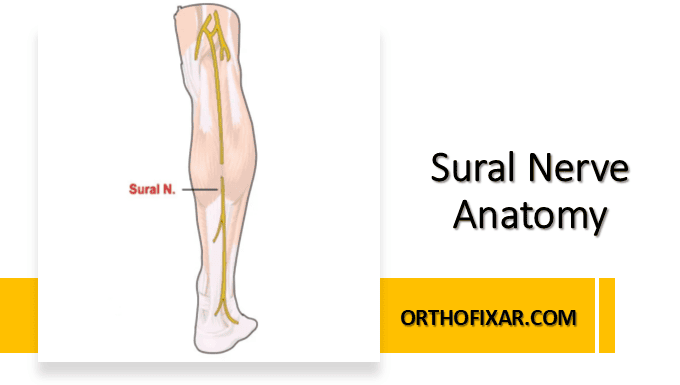
Sural Nerve Origin and Course
The sural nerve originates approximately 8-12 centimeters proximal to the lateral malleolus through the convergence of its two primary components. The medial sural cutaneous nerve branches from the tibial nerve in the popliteal fossa, while the lateral sural cutaneous nerve derives from the common fibular nerve near the fibular head.
See Also: Common Peroneal Nerve Anatomy
The formation of the sural nerve occurs through a complex process of neural migration and fasciculation that typically completes by the second trimester of fetal development. This embryological foundation influences both the nerve’s anatomical course and its susceptibility to various pathological conditions encountered in clinical medicine.
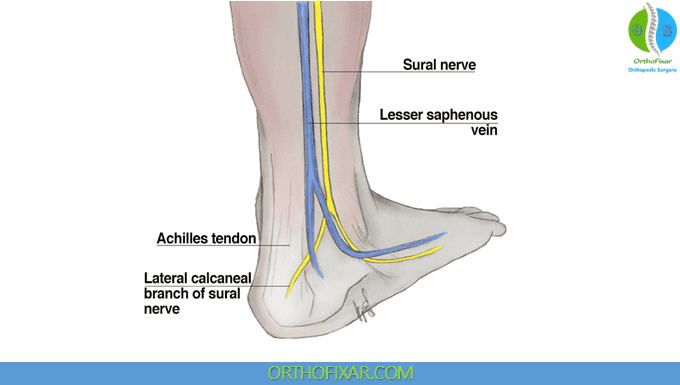
Following its formation, the sural nerve travels in a relatively superficial plane along the posterior aspect of the leg. It courses between the two heads of the gastrocnemius muscle initially, then progresses distally along the lateral border of the Achilles tendon. This superficial location makes the nerve particularly accessible for both diagnostic procedures and surgical interventions.
The nerve continues its descent along the posterior-lateral aspect of the lower leg, maintaining its position between the lateral malleolus and the Achilles tendon. As it approaches the ankle region, the sural nerve becomes increasingly superficial, lying just beneath the skin and superficial fascia.
Anatomical Variations and Clinical Implications
Significant anatomical variations in sural nerve formation occur in approximately 15-20% of the population, presenting important considerations for medical professionals. The most common variation involves incomplete fusion of the medial and lateral components, resulting in dual innervation patterns that can complicate both diagnostic testing and surgical planning.
In some individuals, the lateral sural cutaneous nerve may provide the primary sensory innervation without significant contribution from the medial component. Conversely, other patients may demonstrate predominant medial sural cutaneous nerve innervation with minimal lateral component contribution. These variations can significantly impact nerve conduction studies and must be considered when interpreting electrophysiological data.
Additional anatomical variations include aberrant branching patterns, unusual communication with adjacent nerves, and variations in the precise location of nerve formation. Understanding these variations is crucial for accurate diagnosis of peripheral neuropathies and successful execution of nerve grafting procedures.
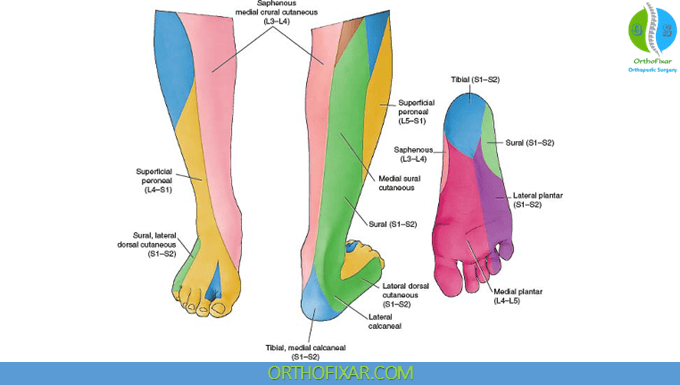
Sensory Distribution and Innervation Territory
The sural nerve provides sensory innervation to a well-defined territory encompassing the lateral aspect of the foot and the posterior-lateral portion of the distal leg. Specifically, the nerve innervates the skin overlying the lateral malleolus, the lateral border of the foot extending to the fifth toe, and a portion of the lateral dorsal foot surface.
The sensory territory of the sural nerve demonstrates some degree of overlap with adjacent sensory nerves, particularly the superficial fibular nerve and the medial plantar nerve. This overlap provides redundancy in sensory innervation but can also complicate the assessment of isolated sural nerve pathology during clinical examination.
Understanding the precise sensory distribution is essential for accurate neurological assessment and for predicting the functional impact of sural nerve injuries or surgical procedures. The nerve’s sensory territory is particularly important in diabetic patients, where sural nerve dysfunction often represents an early manifestation of peripheral neuropathy.
Relationship to Surrounding Anatomical Structures
The sural nerve maintains important anatomical relationships with several key structures throughout its course. In the proximal leg, the nerve lies in close proximity to the small saphenous vein, sharing a common fascial plane that facilitates surgical exposure during nerve grafting procedures.
As the nerve descends, it maintains a consistent relationship with the lateral border of the Achilles tendon, providing a reliable anatomical landmark for surgical identification. The nerve’s superficial location in the distal leg places it at risk during procedures involving the posterior-lateral ankle region, including arthroscopic surgery and fracture fixation.
The sural nerve’s relationship to the lateral malleolus is particularly clinically relevant, as this region represents a common site for both traumatic injury and surgical intervention. The nerve’s proximity to the peroneal tendons and the calcaneofibular ligament must be considered during lateral ankle procedures to prevent iatrogenic injury.
Blood Supply and Vascular Anatomy
The sural nerve receives its blood supply through a segmental pattern of small perforating vessels derived from adjacent muscular and cutaneous arteries. The primary vascular supply originates from branches of the posterior tibial artery, the peroneal artery, and smaller vessels associated with the gastrocnemius and soleus muscles.
This segmental vascular pattern provides redundancy in blood supply, contributing to the nerve’s resilience and making it suitable for grafting procedures. However, the relatively sparse intraneural vasculature compared to mixed nerves may contribute to the sural nerve’s susceptibility to ischemic injury in certain pathological conditions.
Understanding the vascular anatomy is crucial for surgical procedures involving sural nerve harvest, as preservation of the blood supply to remaining nerve segments helps prevent complications such as painful neuromas or persistent sensory deficits.
Surgical Applications and Nerve Grafting
The sural nerve represents the gold standard for autologous nerve grafting procedures due to its consistent anatomy, adequate length, and acceptable donor site morbidity. Surgeons frequently harvest segments of the sural nerve for reconstruction of more critical nerve defects, particularly involving the median, ulnar, or facial nerves.
The nerve’s length, typically 30-40 centimeters when fully mobilized, provides sufficient graft material for most reconstructive procedures. The relatively minor sensory deficit resulting from sural nerve harvest makes it an acceptable trade-off for restoration of more critical nerve function.
Harvesting techniques have evolved to minimize donor site morbidity, with minimally invasive approaches reducing scarring and improving cosmetic outcomes. Understanding the nerve’s anatomical course and relationships is essential for safe and effective harvest procedures.
Pathological Conditions and Clinical Disorders
Several pathological conditions can affect the sural nerve, ranging from traumatic injuries to systemic neuropathies. Diabetic peripheral neuropathy commonly involves the sural nerve, often presenting as one of the earliest manifestations of diabetic complications.
Traumatic injuries to the sural nerve may occur during ankle fractures, particularly those involving the lateral malleolus or during surgical procedures in the posterior-lateral ankle region. These injuries can result in permanent sensory loss and, occasionally, painful neuropathic symptoms.
Other conditions affecting the sural nerve include peripheral nerve tumors, compression syndromes, and inflammatory neuropathies. Understanding the nerve’s anatomy is crucial for accurate diagnosis and appropriate treatment of these conditions.
Resources
- Clinically Oriented Anatomy by Moore, Dalley, and Agur
- Miniato MA, Nedeff N. Anatomy, Bony Pelvis and Lower Limb: Sural Nerve. [Updated 2023 Nov 2]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK546638/