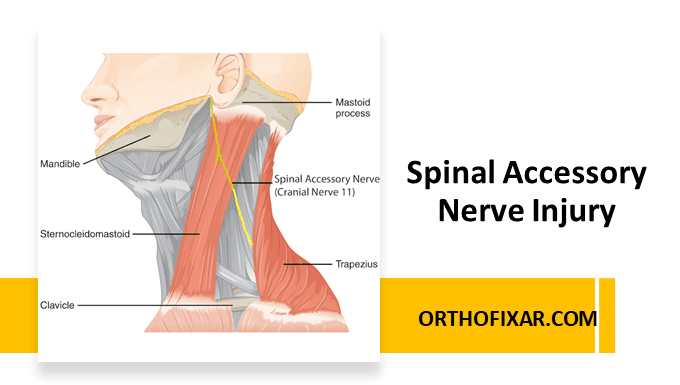
The spinal accessory nerve (cranial nerve XI) is a motor nerve that innervates the sternocleidomastoid and trapezius muscles. This nerve has both cranial and spinal components, with the spinal portion arising from the upper cervical spinal cord segments (C1-C5, predominantly C3-C4).
Spinal accessory nerve injury can result from various causes, with both traumatic and iatrogenic origins being common. It is vulnerable to traumatic injury as it passes the posterior triangle of the neck
Anatomical Considerations
The spinal accessory nerve follows a superficial course through the posterior triangle of the neck, making it particularly vulnerable to traumatic injury. This anatomical pathway places the nerve at risk during surgical procedures in the neck region, particularly lymph node biopsies and neck dissections, as well as from external trauma.
The nerve’s superficial location in the posterior triangle means it lacks the protective coverage of deeper anatomical structures, contributing to its susceptibility to injury from relatively minor trauma or sustained pressure.
See Also: Brachial Plexus Anatomy

Mechanism of Injury
Spinal accessory nerve injury can result from various causes including traumatic and iatrogenic causes. The most common cause for accessory nerve injury is iatrogenic, such as lymph node biopsies that involve the posterior triangle of the neck, neck surgeries including removal of a tumor, carotid or internal jugular vein surgeries, neck dissection (including radical, selective, and modified), or cosmetic surgery (facelift) from the mechanical stress exerted on the neck due to positioning throughout the procedure.
A frequently overlooked cause is chronic pressure from poorly fitting backpacks, where sustained compression over the posterior triangle region can lead to nerve dysfunction. This mechanism is most common in students, hikers, and military personnel who carry heavy loads regularly.
Other common causes include surgical complications during neck procedures (iatrogenic injury), penetrating trauma to the neck region, and stretch injuries from sudden neck movements or positioning during medical procedures.
Clinical Presentation
The clinical presentation of spinal accessory nerve injury is distinctive and directly relates to the nerve’s innervation pattern. Importantly, injury to the spinal accessory nerve typically spares the sternocleidomastoid muscle function, as this muscle receives dual innervation from both the spinal accessory nerve and cervical nerve roots. The primary clinical manifestations therefore involve trapezius muscle dysfunction.
Clinical Signs & Symptoms
Shoulder Drooping: The affected shoulder appears lower than the contralateral side due to loss of trapezius muscle support. The scapula becomes translated laterally and rotates downward, creating an asymmetric shoulder line that is readily apparent on visual inspection.

Scapular Winging: The medial superior portion of the scapula becomes prominent, with medial rotation of the inferior angle. This winging is particularly pronounced during arm abduction movements, as noted by Safran’s observation that spinal accessory palsy results in scapular winging on abduction but not on forward flexion.

Supraclavicular Fossa Changes: Deepening of the supraclavicular fossa occurs as a result of trapezius and the sternocleidomastoid muscle wasting, creating an asymmetric neck-line that becomes more pronounced over time.

Patients with spinal accessory nerve injury experience significant functional impairment, particularly in overhead activities. The most notable limitation is difficulty abducting the arm above 90 degrees. This restriction occurs because the trapezius muscle, particularly its upper and middle fibers, plays a crucial role in scapular stabilization and upward rotation during arm elevation.
The loss of trapezius function disrupts the normal scapulohumeral rhythm, leading to compensatory movement patterns that may result in secondary shoulder pathology if not addressed promptly.
Spinal Accessory Nerve Injury Diagnosis
Diagnosis of spinal accessory nerve injury relies heavily on clinical examination findings, supplemented by appropriate diagnostic studies when indicated. The distinctive pattern of shoulder drooping, scapular winging, and functional limitations in overhead activities should raise suspicion for this condition.
Physical examination should include assessment of shoulder symmetry, scapular positioning and movement, and functional testing of arm elevation. The characteristic finding of scapular winging that is prominent during abduction but not forward flexion is particularly diagnostic.
Electromyography and nerve conduction studies can provide objective confirmation of nerve dysfunction and help assess the severity and prognosis of the injury.
See Also: Scapular Winging Test
Management Implications
Early recognition of spinal accessory nerve injury allows for prompt intervention, which may include physical therapy focused on compensatory strengthening, surgical nerve repair in cases of complete transection, or nerve grafting procedures when indicated.
The prognosis varies depending on the mechanism and severity of injury, with compression injuries generally having a better outcome than complete transection. Patient education regarding activity modification and ergonomic considerations, particularly in cases related to backpack use, is an important component of comprehensive care.
Differential Diagnosis
The differential diagnoses for accessory nerve injury include the following
- Long thoracic nerve injuries that cause paralysis or weakness of the serratus anterior muscle present as winging of the scapula, which is worse with lift-forward arm flexion or pushing the outstretched arm against a wall. This is different from accessory nerve injury, which has winging of the scapula with the abduction of the arm
- Rotator cuff injury has a similar presentation when lifting the arm behind the head, except this injury does not present with winging of the scapula
- Shoulder girdle arthritis and pain syndrome do not have muscular atrophy and winging of the scapula
- Whiplash injury could cause neck pain, cervical spine rigidity, and limited neck motion secondary to spasms and pain
References & More
- AlShareef S, Newton BW. Accessory Nerve Injury. [Updated 2022 Dec 19]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: Pubmed
- Aval SM, Durand P, Shankwiler JA. Neurovascular injuries to the athlete’s shoulder: part I. J Am Acad Orthop Surg. 2007;15:249–256. Pubmed
- Patten C, Hillel AD. The 11th nerve syndrome: accessory nerve palsy or adhesive capsulitis. Arch Otolaryngol Head Neck Surg. 1993;119:215–220. Pubmed
- Wiater JM, Bigliani LU. Spinal accessory nerve injury. Clin Orthop Relat Res. 1999 Nov;(368):5-16. PMID: 10613148. Pubmed