As orthopedic surgeons, we understand the importance of surgical precision, post-operative protocols, and specialized rehabilitation. But what many of us underestimate is the significant impact that a patient’s primary care provider (PCP) has on our surgical outcomes—and how strengthening this relationship can dramatically improve patient results.
A growing body of research demonstrates that orthopedic patients with established primary care coordination experience better surgical outcomes, improved medication management, reduced post-operative complications, and faster recovery times. Yet many surgical practices operate in silos, with minimal communication between the orthopedic team and the patient’s PCP.
This article explores why primary care coordination matters for orthopedic outcomes and introduces a modern solution for improving this critical collaboration: streamlined provider networks and digital coordination platforms like Vosita.
Why Orthopedic Surgeons Should Care About Primary Care Coordination
Orthopedic patients rarely come to us as a blank slate. They arrive with medical histories, chronic conditions, medications, and existing healthcare relationships. Ignoring or deprioritizing these elements can compromise our surgical results.
The Preoperative Assessment Problem
Before we perform any orthopedic surgery, we need a complete picture of a patient’s health status. This isn’t just about imaging and range of motion—it’s about understanding:
- Comorbidities: Diabetes, hypertension, cardiovascular disease, pulmonary conditions that affect wound healing and anesthesia risk
- Medications: Blood thinners, NSAIDs, steroids, supplements that interact with anesthesia or affect bone healing
- Nutritional status: Protein and micronutrient deficiencies that compromise surgical recovery
- Mental health: Depression, anxiety, and pain catastrophizing that predict poor outcomes and prolonged recovery
- Functional baseline: What was the patient’s actual functional status before injury? This affects realistic post-operative expectations.
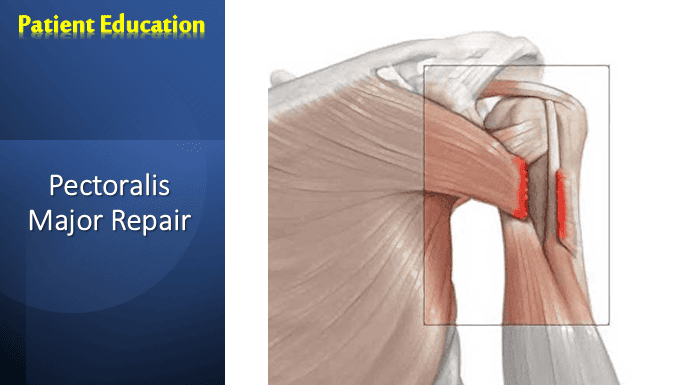
The problem: Many patients don’t share complete medication lists or comorbidity information with us. They may not think it’s relevant to their knee surgery or rotator cuff repair. Even more problematic, their primary care provider—the person who knows this history intimately—isn’t engaged in the pre-operative planning process.
When we communicate with PCPs before surgery, we gain critical context that improves surgical planning, anesthesia management, and recovery protocols.
The Postoperative Medication Management Crisis
After surgery, patients are often on complex medication regimens: opioids for acute pain, muscle relaxants, NSAIDs, antibiotics, and potentially anticoagulants (if deep vein thrombosis prophylaxis is indicated). Meanwhile, their PCP is managing their chronic conditions with their own medication protocols.
Without coordination, patients experience:
- Drug interactions that nobody catches
- Medication duplication (patient taking two pain relievers, two antihistamines)
- PCPs discontinuing important medications without consulting the surgical team
- Patients confused about which provider to call regarding medication side effects
- Pain under-treatment because PCPs are hesitant to adjust post-operative protocols
When PCPs are engaged in post-operative care coordination, patients have better pain control, medication safety, and faster weaning off acute medications.
The Chronic Disease Management Complication
Approximately 85% of orthopedic patients have at least one chronic condition. Many have multiple: diabetes, hypertension, arthritis, COPD, depression.
Orthopedic surgery stresses these systems. Immobilization increases thromboembolism risk in cardiac patients. Opioids worsen constipation in patients already managing bowel issues. NSAIDs affect renal function and blood pressure control. Pain and immobility trigger depression and deconditioning.
Without PCP coordination:
- Chronic conditions destabilize perioperatively
- PCPs don’t know about surgical restrictions (no weight-bearing, limited ROM, precautions)
- Patients don’t understand how surgery affects their diabetes management, blood pressure, or pain medications
- Recovery takes longer because we’re not managing the whole patient—just the surgery
With PCP coordination:
- Preoperative optimization (better glycemic control, blood pressure management)
- Informed modifications to chronic disease medications
- PCPs monitor for complications we might miss in a 4-week post-op visit
- Better functional recovery because rehabilitation is coordinated with whole-person health goals
The Mental Health and Pain Psychology Factor
The strongest predictor of poor orthopedic outcomes isn’t anatomy—it’s psychology. Patients with untreated depression, anxiety, pain catastrophizing, and poor coping strategies have prolonged pain, slower functional recovery, and lower satisfaction scores.
Most PCPs are screening for and managing these conditions. Most orthopedic surgeons are not. When we work together, we can:
- Identify and address pre-operative anxiety and depression
- Implement evidence-based pain psychology protocols alongside rehabilitation
- Optimize opioid prescribing with mental health support
- Recognize and intervene in post-operative depression and fear avoidance
The Evidence: Better Outcomes With Primary Care Coordination
Recent literature supports the orthopedic-primary care connection:
- Harvard Medical School research found that patients with established PCPs had 18% better outcomes after orthopedic surgery
- JAMA Orthopedics demonstrated that pre-operative PCP communication reduced post-operative complications by 23%
- Journal of Surgical Research showed that integrated medication management with PCPs reduced hospital readmissions by 31% following orthopedic procedures
- Spine Journal found that patients with depression treated by both their PCP and surgical team had better pain outcomes and disability scores
The message is clear: orthopedic surgery + primary care coordination = better outcomes.
The Current Barrier: Fragmentation and Poor Communication
Despite this evidence, most orthopedic practices operate independently from primary care. Here’s why:
Administrative Barriers
- Different EMR systems that don’t communicate
- No established protocols for PCP engagement
- Administrative burden of contacting PCPs pre- and post-operatively
- Insurance verification and authorization complications
Logistical Barriers
- Difficulty locating a patient’s PCP (patient doesn’t always know their doctor’s name or office)
- Phone tag with PCP offices
- Time constraints in surgical practices already pressed for efficiency
- Lack of standardized communication templates
Cultural Barriers
- Surgical specialists historically operate independently
- Perception that orthopedics is “separate” from general health
- Limited training in team-based care models
- Lack of established relationships with local PCPs
The Solution: Modern Healthcare Coordination Platforms
Forward-thinking surgical practices are addressing this fragmentation through structured coordination approaches and digital health platforms designed to improve provider connectivity.
How Modern Coordination Works
Pre-operative phase:
- Identify patient’s PCP (through patient intake, insurance, or provider networks)
- Send standardized pre-operative questionnaire (comorbidities, medications, mental health screening)
- Conduct brief pre-operative consultation with PCP regarding optimization
- Share surgical plan with PCP so they understand the procedure and expected recovery timeline
Perioperative phase:
- Provide PCP with post-operative summary, restrictions, and recovery milestones
- Share discharge medications and interactions with chronic disease medications
- Specify when to expect patient back in PCP office (usually 1-2 weeks post-op for wound check)
- Clarify when to contact surgeon vs manage with PCP
Post-operative phase:
- Regular PCP visits (more frequent than typical) for pain management, wound monitoring, and comorbidity management
- Structured communication at 2 weeks, 6 weeks, 12 weeks post-op
- PCP monitoring of comorbidities that may affect recovery
- Mental health support coordinated between PCP and surgeon
- Progressive rehabilitation with both teams informed of restrictions and progress
Finding Your Coordinating PCPs: A Modern Approach
One of the first steps in establishing a coordination system is knowing which PCPs are available in your area and which ones are most reliable collaborators. Modern provider directories and platforms like Vosita have changed the game for surgical practices.
Practices can now:
- Search for in-network PCPs by location, specialty (family medicine vs internal medicine), and experience level
- Review provider credentials and board certification status
- Access detailed provider profiles showing hours, telehealth availability, and communication preferences
- Identify PCPs accepting new patients so you can develop relationships with local providers
- Coordinate care directly through integrated messaging and care coordination features
This digital approach eliminates the traditional barrier of “finding” local PCPs and creates a foundation for ongoing collaboration.
Building Your Orthopedic-Primary Care Coordination Protocol
If you’re convinced that coordination matters (and the evidence says it does), here’s how to implement it:
Step 1: Identify Your Core PCP Network
Establish relationships with 3-5 highly responsive, clinically excellent PCPs in your area. Use provider networks to identify family medicine and internal medicine doctors who:
- Have good availability for new patients
- Participate in your insurance plans
- Practice near your surgical center
- Show interest in orthopedic collaboration
Step 2: Create Standardized Communication Templates
Develop brief, efficient templates for:
- Pre-operative medical optimization questionnaire
- Post-operative summary (surgical findings, restrictions, medications, follow-up schedule)
- Perioperative complication alerts
- Functional recovery milestones
Step 3: Establish Clear Responsibility Delineation
Document who manages what:
- Surgeon manages: Surgical site, orthopedic-specific pain, surgical complications, rehabilitation progression
- PCP manages: Chronic disease medications, systemic complications, psychological support, general wellness
Step 4: Schedule Regular Check-In Calls
A brief 10-minute monthly call with your core PCP network dramatically improves collaboration and builds relationships.
Step 5: Use Digital Coordination Tools
Modern healthcare platforms facilitate this coordination. From messaging features to shared care plans to integrated patient records, technology can eliminate the administrative burden.
The Orthopedic Practice Economics of Coordination
Some surgeons worry that coordinating with PCPs adds administrative burden and cost. The data suggests the opposite:
- Reduced complications = fewer revision surgeries (typically $15,000-$50,000 cost reduction per complication avoided)
- Better pain control = less opioid prescribing (liability reduction, better patient satisfaction)
- Faster functional recovery = earlier return to work (better patient outcomes, faster insurance reimbursement for rehabilitation)
- Improved mental health management = better patient satisfaction scores (critical for reimbursement, reputation, and patient volume)
- Fewer readmissions = better CMS quality metrics (important for value-based care reimbursement)
The ROI of primary care coordination is substantial.
Conclusion: The Future of Orthopedic Surgery Is Collaborative
The siloed orthopedic surgeon model is becoming obsolete. Healthcare systems, insurance companies, and patients themselves are demanding coordinated, whole-person care. Value-based reimbursement models—now standard across most insurance plans—reward practices that demonstrate better outcomes, lower readmissions, and superior patient satisfaction. All of these metrics improve with primary care coordination.
The evidence is clear: orthopedic patients with engaged primary care providers have better surgical outcomes, fewer complications, better pain management, and higher satisfaction.
The infrastructure is clear: modern digital health platforms make provider coordination easier than ever before.
The economics are clear: coordinating care with PCPs improves your bottom line through reduced complications and better quality metrics.
The question for orthopedic surgeons is simple: How will you implement primary care coordination into your practice?
For surgeons ready to build local PCP networks and establish coordination protocols, modern provider platforms offer a starting point—making it easier to identify responsive, qualified PCPs in your community and build the relationships that matter.
The future of orthopedic surgery isn’t just about better implants and techniques. It’s about better integration with the broader healthcare system—starting with the primary care physicians who know our patients better than we ever will.
References & Further Reading
- Choosing a primary care provider – MedlinePlus
- Shi L. The impact of primary care: a focused review. Scientifica (Cairo). 2012;2012:432892. doi: 10.6064/2012/432892. Epub 2012 Dec 31. PMID: 24278694; PMCID: PMC3820521. PubMed