For the orthopedic specialist, anatomical knowledge is not an academic exercise—it’s the foundation of every diagnosis, surgical plan, and clinical decision. While the basics are long-mastered, the challenge lies in retaining the vast, three-dimensional details of the musculoskeletal system and applying that knowledge under pressure. This guide moves beyond general study tips to offer clinically-focused strategies for mastering the intricate anatomy essential to our practice.
Beyond the Atlas: Integrating Anatomy with Surgical Approaches
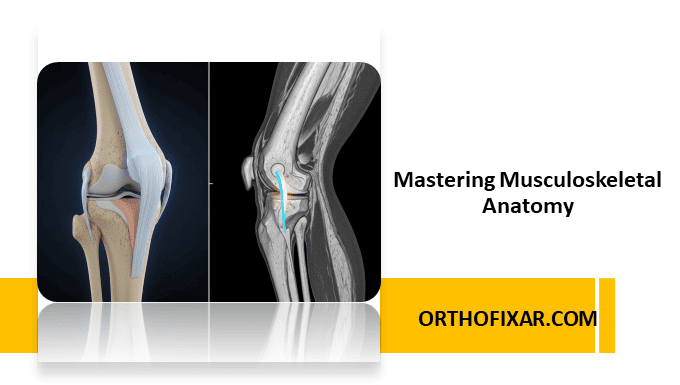
Static diagrams are insufficient for surgical application. True mastery comes from visualizing anatomy in the context of function and procedure. Instead of just memorizing structures, link them directly to their surgical relevance.
1. Procedural Visualization and Surgical Windows
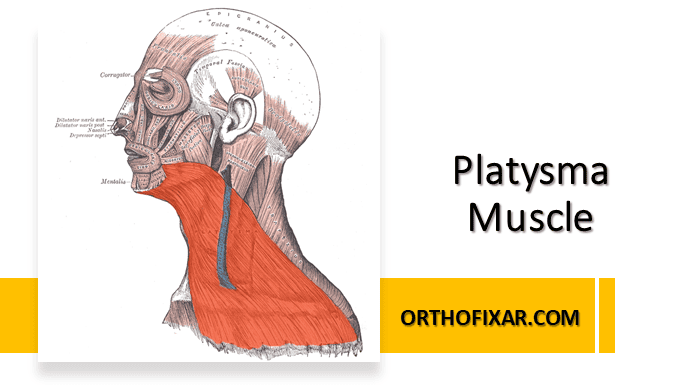
Don’t just learn the location of the axillary nerve. Visualize its course during a lateral approach to the shoulder and identify the precise safe zone for your incision. This mental rehearsal can be powerfully augmented by viewing detailed 3D surgical animations that demonstrate a procedure from start to finish, clarifying the dynamic relationship between instruments, retractors, and anatomy. Think of your surgical approaches as navigating through specific ‘anatomical windows.’ When studying the femoral triangle, see it as the gateway for the anterior approach to the hip, treating the femoral artery, vein, and nerve not as abstract points, but as structures to be meticulously protected.
2. Correlate with Cross-Sectional and Variant Anatomy
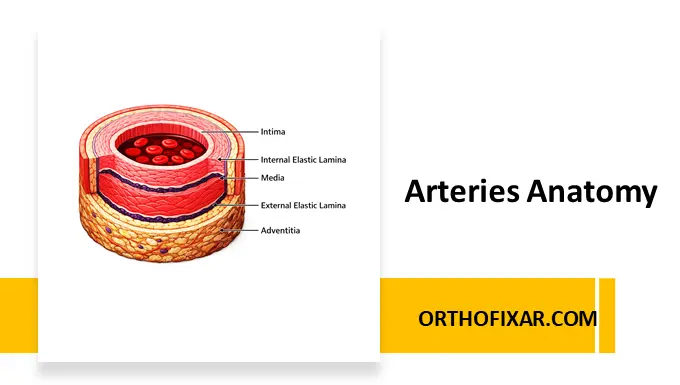
Beyond 3D models, proficiency in interpreting cross-sectional anatomy from MRI and CT scans is essential. Regularly correlate your 3D anatomical understanding with axial, sagittal, and coronal imaging slices. This skill is invaluable for pre-operative planning, allowing you to anticipate challenges. Furthermore, a true master of anatomy is prepared for common anatomical variations. Be aware of potential differences in the branching pattern of the brachial plexus or the course of the sciatic nerve relative to the piriformis. Anticipating these variants moves knowledge from theoretical to practical, preparing you for intraoperative realities.

3. Leverage Specialist Tools and Haptic Learning
Move beyond general anatomy apps. For interactive exploration of pathologies, from complex fracture patterns to post-surgical repairs with hardware, platforms like VOKA 3D Anatomy and Pathology’s provide invaluable, manipulable 3D models of traumatology and orthopedics.

3D Model of Extraarticular Comminuted Fracture of Acromial End of Clavicle from VOKA 3D Anatomy & Pathology
Supplement this with professional-level resources like AO Surgery Reference or specialized texts such as Netter’s Concise Orthopaedic Anatomy. To bridge the gap between visualization and the tactile sensations of surgery, incorporate haptic and kinesthetic learning. Engage with surgical simulation platforms like Touch Surgery or participate in cadaveric labs. These tools help develop a muscle memory for navigating anatomical planes and identifying structures by feel, a skill that diagrams alone cannot teach.
Active Recall for the Clinic and the OR
In orthopedics, recall must be instantaneous. Active recall, the process of deliberately retrieving information from memory, is a critical skill for building the rapid, accurate knowledge base required in clinical settings.
Frame your recall practice around clinical scenarios:
- For Diagnosis: When a patient presents with a foot drop, actively recall the muscles of the anterior compartment of the leg, their innervation (Deep Peroneal Nerve), and the corresponding nerve roots (L4, L5) to immediately begin constructing your differential diagnosis.
- For Trauma: When analyzing a radiograph of a distal humerus fracture, actively recall the surrounding neurovascular structures—the brachial artery, median nerve, and ulnar nerve—and their precise locations relative to the bone fragments to anticipate potential complications. This practice converts static knowledge into an active diagnostic skill.
High-Yield Mnemonics for the Orthopedic Specialist
Mnemonics are efficient tools for encoding complex information. Focus on those with the highest clinical utility in orthopedics.
- Brachial Plexus Branches: Really Tired? Drink Coffee Black. (Roots, Trunks, Divisions, Cords, Branches).
- Rotator Cuff Muscles: SITS (Supraspinatus, Infraspinatus, Teres Minor, Subscapularis).
- Carpal Bones (Proximal to Distal, Radial to Ulnar): So Long To Pinky, Here Comes The Thumb. (Scaphoid, Lunate, Triquetrum, Pisiform, Hamate, Capitate, Trapezoid, Trapezium).
Fusing Anatomy with Biomechanics
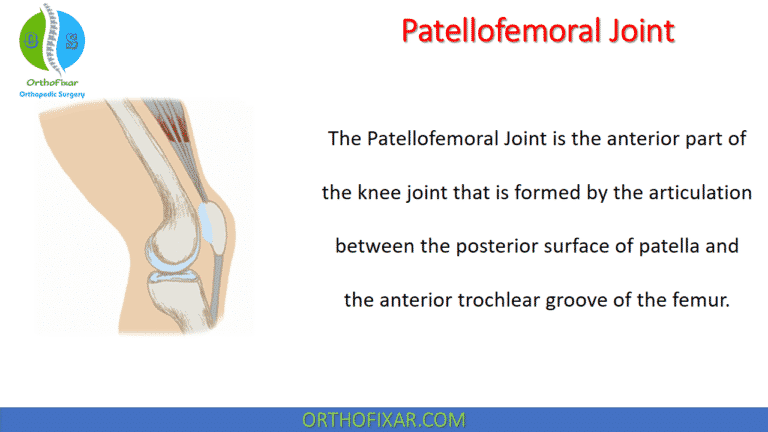
For an orthopedic surgeon, anatomy is inseparable from biomechanics. Understanding the why behind a structure’s design is key to understanding its pathology and treatment. Function dictates form.
When you study a structure, ask why it is built that way. For example, understanding the dense, arched trabecular patterns in the femoral head and neck isn’t just memorization; it’s about understanding how forces are transmitted across the hip joint. This biomechanical insight immediately clarifies why certain fracture patterns, like those through the vulnerable Ward’s triangle, are so common. Connecting form to function makes anatomical knowledge more intuitive and permanent.
Summing Up: A Commitment to Lifelong Learning
For the practicing orthopedic professional, mastering anatomy is a continuous process. By moving beyond basic memorization and adopting clinically-integrated learning strategies, you can develop a deeper, more functional understanding of the musculoskeletal system. Visualizing anatomy through a surgical lens, using active recall for diagnostic challenges, and linking structure to biomechanical function will directly enhance clinical efficacy.
Finally, one of the most effective ways to master a subject is to teach it. Engage in peer-to-peer discussions, mentor junior residents, or explain procedures to medical students. The act of articulating complex anatomical relationships to others will solidify your own knowledge and reinforce these high-yield concepts, ensuring your expertise not only lasts but grows.