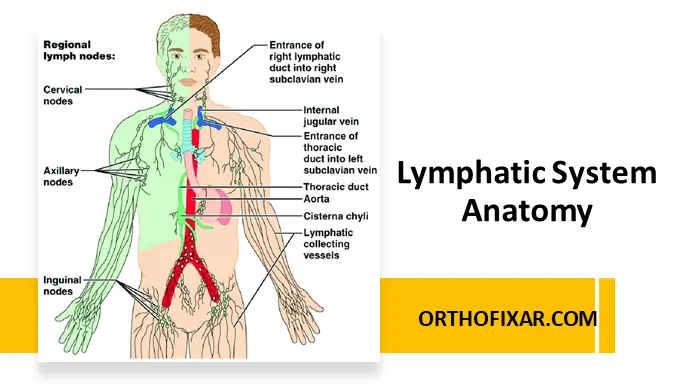
The lymphatic system is an extensive vascular drainage network that collects excess interstitial fluid, plasma proteins, cellular debris, and immune cells from body tissues and returns them to the venous circulation. Beyond fluid balance, it plays a central role in immune defense, inflammation control, and disease surveillance.
Anatomically and functionally, the lymphatic system works in close coordination with the cardiovascular and immune systems. Disruption of lymphatic flow leads to clinically significant conditions such as lymphedema, recurrent infections, and impaired immune responses.
Components of the Lymphatic System
1. Lymphatic Capillaries
Lymphatic capillaries originate blindly within the extracellular (interstitial) spaces of most tissues. Unlike blood capillaries, they have:
- Highly porous endothelial walls
- No basement membrane
- One-way overlapping endothelial “flaps”
This unique structure allows lymphatic capillaries to absorb:
- Tissue fluid
- Plasma proteins
- Cells and cellular debris
- Microorganisms
These microscopic vessels form dense lymphatic plexuses, particularly in the skin, gastrointestinal tract, lungs, and connective tissues.
2. Collecting Vessels and Lymphatic Ducts
From the capillary networks, lymph flows centrally through:
- Collecting lymphatic vessels
- Lymphatic trunks
- Major lymphatic ducts
These vessels contain valves to maintain unidirectional flow and rely on skeletal muscle contraction, arterial pulsation, and respiratory movements to propel lymph.
Major Lymphatic Ducts
Right Lymphatic Duct
- Drains:
- Right side of the head and neck
- Right thorax
- Right upper limb
- Empties into:
- Junction of the right internal jugular vein and right subclavian vein
Thoracic Duct
- Largest lymphatic vessel in the body
- Drains:
- Both lower limbs
- Abdomen
- Left thorax
- Left upper limb
- Left side of head and neck
- Empties into:
- Junction of the left internal jugular vein and left subclavian vein
See Also: Veins Anatomy: Structure, Function, and Clinical Importance
Lymph Nodes: Anatomy and Function
Structural Characteristics
Lymph nodes are encapsulated, round to bean-shaped structures that vary in size and location:
- Preauricular nodes: very small, often barely palpable
- Inguinal nodes: commonly 1–2 cm in adults
They are strategically positioned along lymphatic vessels to act as biological filters.
Immunological Role
Within lymph nodes:
- Macrophages engulf bacteria and cellular debris
- Lymphocytes (B and T cells) initiate immune responses
- Antibodies are produced
This makes lymph nodes critical for infection control, cancer surveillance, and immune memory. Numerous immunology studies indexed on PubMed confirm the lymph node’s role as a primary site for antigen presentation and lymphocyte activation.
Superficial Lymph Nodes and Clinical Examination
Only superficial lymph nodes are accessible during physical examination. These include:
- Cervical lymph nodes
- Axillary lymph nodes
- Epitrochlear lymph nodes
- Inguinal lymph nodes
Their size, tenderness, consistency, and mobility provide essential diagnostic clues in infection, malignancy, and systemic disease.
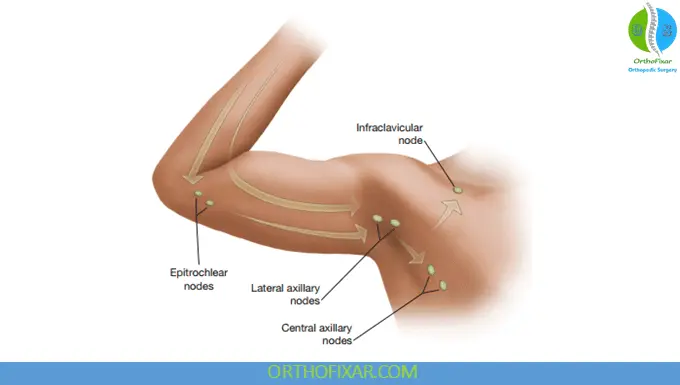
Upper Limb Lymphatic Drainage
Axillary Nodes
The axillary lymph nodes drain most of the upper limb and are the primary nodes examined in routine practice.
Epitrochlear Nodes
- Located on the medial arm, approximately 3 cm above the elbow
- Drain lymph from:
- Ulnar surface of forearm and hand
- Little finger
- Ring finger
- Adjacent side of the middle finger
Enlargement of epitrochlear nodes is always abnormal in adults and often indicates infection or systemic disease.
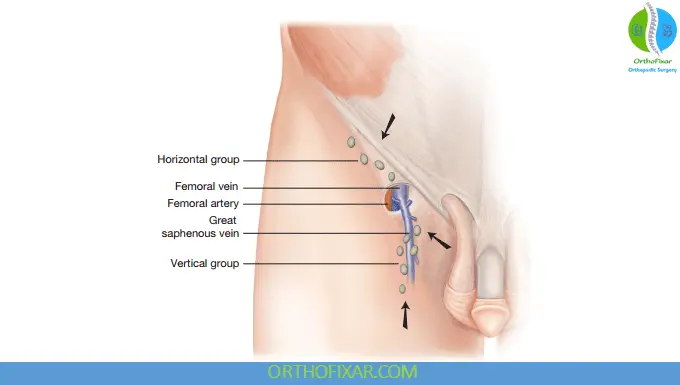
Lower Limb Lymphatic Drainage
The lymphatics of the lower limb follow venous pathways and are divided into:
Superficial System (Palpable)
Superficial Inguinal Lymph Nodes
- Horizontal group
- Drains:
- Lower abdominal wall
- Buttocks
- External genitalia (excluding testes)
- Anal canal and perianal region
- Lower vagina
- Drains:
- Vertical group
- Located along the great saphenous vein
- Drains superficial tissues of the leg
Deep System (Not Palpable)
- Lymphatics accompanying deep veins
- Drain into deep inguinal and iliac nodes
Clinical Note:
Lymph from the heel and lateral foot (small saphenous vein territory) enters the deep system at the popliteal fossa, meaning pathology in this region may not produce palpable inguinal lymphadenopathy—a detail many clinicians miss.
Clinical Importance of the Lymphatic System
The lymphatic system is directly involved in:
- Infection spread and containment
- Cancer metastasis
- Inflammatory and autoimmune diseases
- Post-surgical and post-traumatic edema
Modern anatomical and immunological research published in PubMed-indexed journals continues to highlight the lymphatic system’s role in tumor immunology, vaccine response, and chronic inflammatory disorders.
Ignoring lymphatic anatomy in clinical practice is a mistake. A costly one.
Key Takeaways
- The lymphatic system maintains fluid balance and immune defense
- Lymphatic capillaries are structurally unique and highly permeable
- Lymph nodes filter lymph and activate immune responses
- Only superficial lymph nodes are clinically palpable
- Understanding drainage patterns prevents diagnostic errors
Final Opinion
If you don’t understand lymphatic anatomy, you will misinterpret swelling, miss early malignancy signs, and misunderstand immune responses. This system deserves the same respect as arteries and nerves—and it’s about time medical education treated it that way.
Comparison Tables
Comparison Table 1: Lymphatic System vs Blood Vascular System
| Feature | Lymphatic System | Blood Vascular System |
|---|---|---|
| Primary Function | Drains excess tissue fluid and supports immunity | Transports oxygen, nutrients, and waste |
| Type of System | One-way drainage system | Closed, continuous circulation |
| Fluid Carried | Lymph (protein-rich interstitial fluid) | Blood |
| Capillary Structure | Highly permeable, no basement membrane | Continuous endothelium with basement membrane |
| Valves | Present in collecting vessels | Present mainly in veins |
| Central Pump | None | Heart |
| Immune Role | Major (lymph nodes, lymphocytes) | Minimal |
| Flow Direction | Tissues → veins | Heart → tissues → heart |
Comparison Table 2: Right Lymphatic Duct vs Thoracic Duct
| Feature | Right Lymphatic Duct | Thoracic Duct |
|---|---|---|
| Size | Short and small | Largest lymphatic vessel |
| Drainage Area | Right head, neck, thorax, upper limb | Rest of the body |
| Entry Point | Right internal jugular–subclavian junction | Left internal jugular–subclavian junction |
| Clinical Importance | Less commonly injured | Frequently involved in trauma/surgery |
| Volume Drained | Minor portion of total lymph | Majority of lymph return |
Comparison Table 3: Lymphatic Capillaries vs Blood Capillaries
| Feature | Lymphatic Capillaries | Blood Capillaries |
|---|---|---|
| Basement Membrane | Absent | Present |
| Endothelial Junctions | Loose, overlapping flaps | Tight junctions |
| Permeability | Very high | Moderate |
| Contents Absorbed | Fluid, proteins, cells, bacteria | Gases, nutrients, waste |
| Flow Direction | One-way | Two-way exchange |
Comparison Table 4: Superficial vs Deep Lymph Nodes
| Feature | Superficial Lymph Nodes | Deep Lymph Nodes |
|---|---|---|
| Palpability | Palpable on exam | Not palpable |
| Location | Subcutaneous tissue | Along deep vessels |
| Examples | Cervical, axillary, inguinal | Iliac, para-aortic |
| Clinical Use | Infection, malignancy screening | Imaging-based assessment |
| Exam Relevance | High | Limited |
Comparison Table 5: Axillary vs Epitrochlear Lymph Nodes
| Feature | Axillary Nodes | Epitrochlear Nodes |
|---|---|---|
| Location | Axilla | Medial arm, ~3 cm above elbow |
| Drainage Area | Most of upper limb | Ulnar forearm, hand, little & ring fingers |
| Normal Palpability | May be palpable | Not normally palpable |
| Clinical Significance | Breast & upper limb pathology | Always abnormal if enlarged |
| Exam Value | High | Very high (red flag node) |
Comparison Table 6: Superficial Inguinal Node Groups
| Feature | Horizontal Group | Vertical Group |
|---|---|---|
| Location | Below inguinal ligament | Along great saphenous vein |
| Drainage | Lower abdomen, buttock, genitalia, perianal region | Superficial leg |
| Clinical Relevance | STI, anal & genital disease | Lower limb infections |
| Palpability | Palpable | Palpable |
Comparison Table 7: Superficial vs Deep Lower Limb Lymphatics
| Feature | Superficial System | Deep System |
|---|---|---|
| Relation to Veins | Follows superficial veins | Follows deep veins |
| Palpability | Yes (inguinal nodes) | No |
| Drainage Path | Skin and subcutaneous tissue | Muscles and joints |
| Key Clinical Note | Commonly enlarged | Lesions may be missed on exam |
| Example Area | Thigh, leg surface | Popliteal region |
References & More
- Elshikh M, Moawad AW, Salem U, Klimkowski SP, Hassan T, Rao Korivi B, Jensen CT, Javadi S, Elsayes KM. Oncologic Imaging of the Lymphatic System: Current Perspective with Multi-Modality Imaging and New Horizon. Cancers (Basel). 2021 Sep 10;13(18):4554. doi: 10.3390/cancers13184554. PMID: 34572781; PMCID: PMC8465736. Pubmed
- Null M, Arbor TC, Agarwal M. Anatomy, Lymphatic System. 2023 Mar 6. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan–. PMID: 30020619. Pubmed
- Null M, Arbor TC, Agarwal M. Anatomy, Lymphatic System. [Updated 2023 Mar 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: Pubmed
- Bickley, L. S., Szilagyi, P. G., Hoffman, R. M., & Soriano, R. P. (2021). Bates’ guide to physical examination and history taking, 12e.
[…] Lymphatic obstruction (e.g., malignancy, filariasis) […]