The common peroneal nerve, also known as the common fibular nerve, represents one of the most clinically significant peripheral nerves in the lower extremity. Understanding its complex anatomy is essential for healthcare providers involved in diagnosing and treating lower limb pathologies, particularly given its vulnerability to injury and its critical role in dorsiflexion and eversion movements.
Common Peroneal Nerve Anatomy
Anatomical Origin and Course
The common peroneal nerve originates as the lateral component of the sciatic nerve bifurcation, typically occurring at the superior angle of the popliteal fossa. This division usually takes place approximately 6-8 centimeters proximal to the popliteal fossa, though anatomical variations exist. The nerve carries fibers from the L4, L5, S1, and S2 nerve roots, inheriting both motor and sensory components that will eventually innervate specific muscle groups and cutaneous territories in the leg and foot.
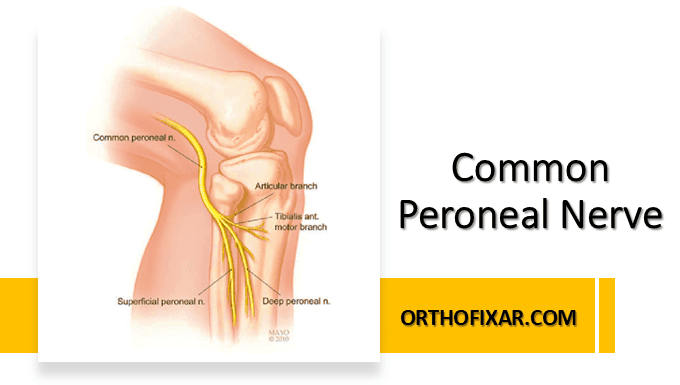
From its origin, the common peroneal nerve follows the medial border of the biceps femoris muscle as it courses laterally and inferiorly through the popliteal fossa. The nerve then travels along the lateral aspect of the knee, passing posterior to the fibular head. This anatomical relationship is particularly significant clinically, as the nerve’s superficial position at the fibular neck makes it susceptible to compression injuries, particularly in patients who experience prolonged pressure or trauma to this region.
See Also: Lumbar Plexus Anatomy
Anatomical Relations and Vulnerable Points
The most clinically relevant anatomical relationship of the common peroneal nerve occurs at the fibular neck, where the nerve winds around the lateral aspect of the fibular head before entering the anterior compartment of the leg. At this location, the nerve lies directly against the bone and is covered only by skin and subcutaneous tissue, making it the most common site of peroneal nerve injury.
The nerve passes through the fibular tunnel, a fibrous arch formed by the origin of the peroneus longus muscle from the fibular head. This tunnel can become a site of nerve entrapment, particularly in cases of muscle hypertrophy, inflammation, or anatomical variations. The proximity of the nerve to the fibular head also explains why fractures involving this bone frequently result in peroneal nerve dysfunction.
Terminal Branches and Distribution
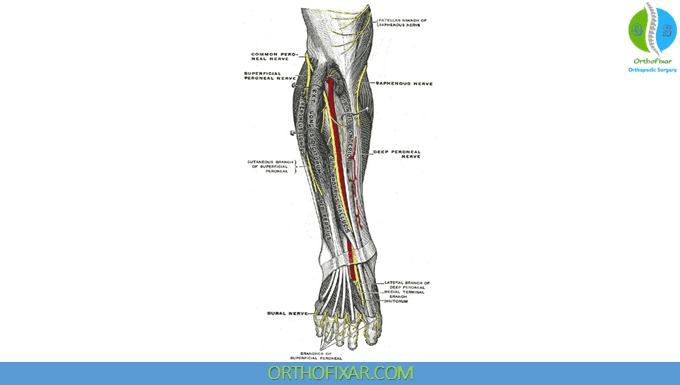
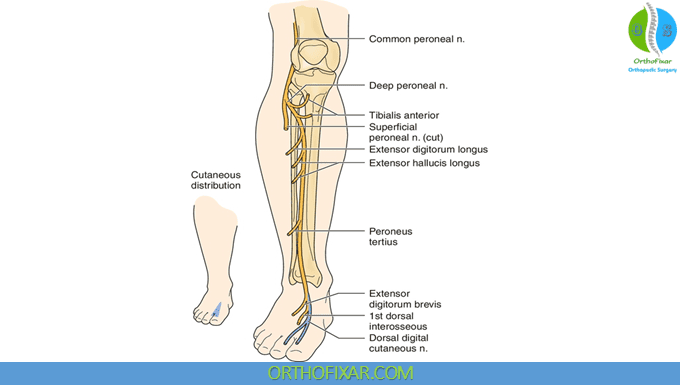
Approximately 2-4 centimeters distal to the fibular head, the common peroneal nerve divides into its two terminal branches: the superficial peroneal nerve and the deep peroneal nerve. This bifurcation typically occurs within the substance of the peroneus longus muscle or at the superior border of the extensor digitorum longus muscle.
The superficial peroneal nerve, also called the superficial fibular nerve, provides motor innervation to the peroneus longus and peroneus brevis muscles, which are responsible for eversion and plantar flexion of the foot. The nerve continues distally through the lateral compartment of the leg before piercing the deep fascia in the lower third of the leg to provide sensory innervation to the dorsum of the foot, excluding the first web space.
The deep peroneal nerve, or deep fibular nerve, travels through the anterior compartment of the leg alongside the anterior tibial artery. This nerve provides motor innervation to the anterior compartment muscles, including the tibialis anterior, extensor hallucis longus, extensor digitorum longus, and peroneus tertius. These muscles are primarily responsible for dorsiflexion of the ankle and extension of the toes. The deep peroneal nerve also supplies sensory innervation to the first web space between the great toe and second toe.
See Also: Sciatic Nerve Anatomy
Clinical Significance and Pathophysiology
The anatomical vulnerability of the common peroneal nerve has significant clinical implications. Peroneal nerve palsy is the most common mononeuropathy in the lower extremity, often resulting from compression at the fibular head. This condition frequently occurs in patients who experience prolonged bed rest, improper positioning during surgery, or direct trauma to the lateral knee region.
Understanding the precise anatomy of the common peroneal nerve is crucial for accurate diagnosis of foot drop, a condition characterized by weakness or paralysis of the dorsiflexor muscles. The anatomical distribution of the nerve’s branches helps clinicians differentiate between common peroneal nerve lesions and other causes of foot drop, such as L5 radiculopathy or central nervous system pathology.
The nerve’s anatomy also plays a critical role in surgical planning, particularly during procedures involving the lateral knee, fibular osteotomy, or compartment release surgeries. Surgeons must maintain awareness of the nerve’s course to prevent iatrogenic injury during these interventions.
Anatomical Variations
Several anatomical variations of the common peroneal nerve have been documented in the literature. The level of sciatic nerve bifurcation can vary significantly, with some individuals demonstrating separation as high as the pelvis or as low as the popliteal fossa. Additionally, the relationship between the nerve and surrounding muscular structures may differ, potentially affecting the nerve’s vulnerability to compression.
Some individuals may present with accessory peroneal nerves or variations in the branching pattern of the terminal divisions. These anatomical variants can influence both the clinical presentation of nerve injuries and the success of surgical interventions aimed at nerve decompression or repair.
Imaging and Diagnostic Considerations
Modern imaging techniques, including high-resolution ultrasound and magnetic resonance neurography, have enhanced our ability to visualize the common peroneal nerve and identify pathological changes. Understanding the normal anatomical course and relationships of the nerve is essential for accurate interpretation of these imaging studies.
Electrophysiological studies, including nerve conduction studies and electromyography, rely heavily on anatomical knowledge for proper electrode placement and interpretation of results. The specific muscle groups innervated by each branch of the common peroneal nerve must be understood to accurately localize lesions and assess the extent of nerve damage.
Surgical Anatomy and Therapeutic Implications
Surgical approaches to the common peroneal nerve require precise anatomical knowledge to ensure successful outcomes. Decompression procedures typically focus on the fibular tunnel region, where the nerve is most commonly entrapped. Understanding the relationship between the nerve and the peroneus longus muscle is crucial for safe surgical exposure and effective decompression.
See Also: Peroneal Nerve Injury

Nerve repair or grafting procedures may be necessary in cases of complete nerve transection or severe injury. The anatomy of the nerve’s branches and their respective target muscles must be thoroughly understood to achieve optimal functional restoration through these complex reconstructive procedures.
The anatomical knowledge of the common peroneal nerve also informs rehabilitation strategies following injury or surgical intervention. Physical therapy protocols must consider the specific muscle groups affected and their functional contributions to normal gait and lower extremity biomechanics.
Understanding the intricate anatomy of the common peroneal nerve remains fundamental to effective clinical practice in orthopedics, neurology, physical medicine and rehabilitation, and related medical specialties. This knowledge directly impacts diagnostic accuracy, treatment planning, and patient outcomes in conditions affecting this clinically significant peripheral nerve.
Resources
- Hardin JM, Devendra S. Anatomy, Bony Pelvis and Lower Limb: Calf Common Peroneal Nerve (Common Fibular Nerve) [Updated 2022 Oct 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532968/
- Wikipedia – Common fibular nerve
Closed.