Arteries are the high‑pressure conduits that deliver oxygen‑rich blood from the heart to the systemic circulation. Understanding the detailed arteries anatomy is crucial for interpreting imaging, performing procedures, and managing vascular diseases.
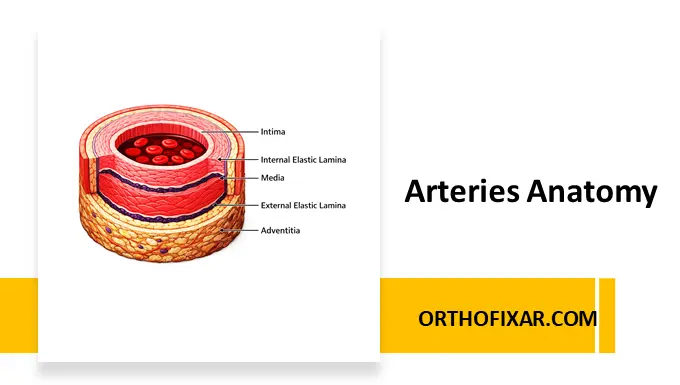
Layers of the Arterial Wall
There are three Concentric Layers of the Arterial Wall:
Intima – The Dynamic Endothelial Lining
The endothelium is not a passive barrier; it is a metabolically active organ. Under physiologic conditions it produces anti‑thrombotic agents (prostacyclin, tissue‑type plasminogen activator) and pro‑thrombotic factors (von Willebrand factor, PAI‑1) in a tightly regulated balance. Dysfunction—often triggered by oxidized LDL, hypertension, or smoking—shifts this equilibrium toward pro‑inflammatory and pro‑thrombotic phenotypes, setting the stage for atherosclerotic plaque initiation.
Clinical pearl: Endothelial dysfunction is the earliest detectable change in patients at risk for coronary artery disease (CAD) and can be assessed non‑invasively via flow‑mediated dilation (FMD).
Media – The Contractile Engine
The media’s smooth‑muscle cells (SMCs) respond to neurohumoral stimuli (e.g., norepinephrine, angiotensin II) and mechanical stretch. Their ability to contract and relax modulates systemic vascular resistance (SVR) and maintains blood pressure homeostasis.
Elastic laminae:
- Internal Elastic Lamina (IEL) separates intima from media.
- External Elastic Lamina (EEL) separates media from adventitia.
Both laminae consist of elastin fibers and are more pronounced in elastic arteries (e.g., aorta) than in muscular arteries (e.g., radial artery).
Adventitia – The Supportive Outer Shell
The adventitia’s collagenous network ensures tensile strength, while its nerve fibers (sympathetic & parasympathetic) regulate vascular tone indirectly. The vasa vasorum—tiny micro‑vessels that originate from the adjacent large arteries—provide essential oxygen and nutrients to the outer media and adventitia, especially in large‑diameter arteries where diffusion alone is insufficient.
Elastic Membranes – Internal & External Elastic Laminae
- Internal elastic membrane (lamina): A thin, fenestrated sheet that allows passage of nutrients and immune cells while providing elastic recoil.
- External elastic membrane (lamina): Less prominent, demarcates media from adventitia in larger arteries and contributes to elastic recoil after systolic stretch.
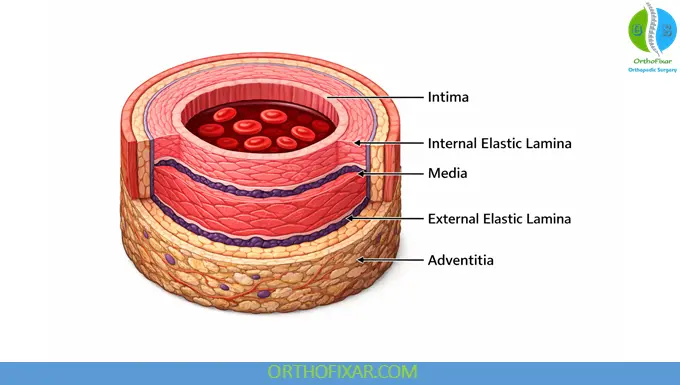
| Layer | Primary Cellular/Extracellular Components | Primary Functions |
|---|---|---|
| Intima (innermost) | Single layer of endothelial cells resting on a thin subendothelial basement membrane; occasional subendothelial connective tissue. | – Regulates thrombosis (prostacyclin, heparin‑like molecules) – Synthesizes vasodilators (NO, prostacyclin) & vasoconstrictors (endothelin, ACE) – Modulates inflammation (interleukins, adhesion molecules) |
| Media (middle) | Smooth‑muscle cells arranged in concentric sheets; abundant elastic fibers forming the internal and external elastic laminae. | – Adjusts vessel diameter via vasoconstriction/vasodilation – Provides structural strength against pulsatile pressure – Hosts vasa vasorum (tiny vessels) that nourish the outer media |
| Adventitia (outer) | Loose connective tissue rich in collagen, nerve fibers, and vasa vasorum. | – Anchors the artery to surrounding structures – Conveys autonomic innervation (sympathetic & parasympathetic fibers) – Supplies nutrients and oxygen to outer vessel wall |
Arterial Branching & Size Gradient
Arteries transition from highly elastic large‑caliber vessels (aorta, common carotid, iliac) to medium‑sized muscular arteries (coronary, renal) and finally to small muscular arteries (<2 mm) and arterioles (20–100 µm). This hierarchy reflects both hemodynamic demands and histologic composition.
| Vessel Type | Typical Diameter | Dominant Wall Component | Primary Physiologic Role |
|---|---|---|---|
| Elastic (e.g., aorta) | 20–30 mm | Prominent elastic laminae, thin media | Dampens pulse‑wave energy, stores systolic energy |
| Muscular (e.g., radial) | 2–5 mm | Thick media with abundant SMCs | Regulates regional blood flow, contributes to systemic resistance |
| Arterioles | 20–100 µm | Thin media, extensive smooth‑muscle tone | Primary site of vascular resistance (Laplace’s law) |
| Capillaries | 7–8 µm | Endothelium only (no media) | Exchange of gases, nutrients, waste |
Resistance is inversely proportional to the fourth power of radius (Poiseuille’s law). Hence arterioles, despite their tiny size, control >70 % of systemic vascular resistance.
Practical tip: When assessing a patient’s blood pressure response to medication, remember that muscular arteries are the primary target for calcium‑channel blockers, whereas arterioles respond to ACE inhibitors via reduced SMC tone.
Palpable Arterial Pulses – Clinical Landmarks
Palpation of arterial pulses remains a cornerstone of physical examination. Below is a quick‑reference guide that can be incorporated into bedside teaching slides.
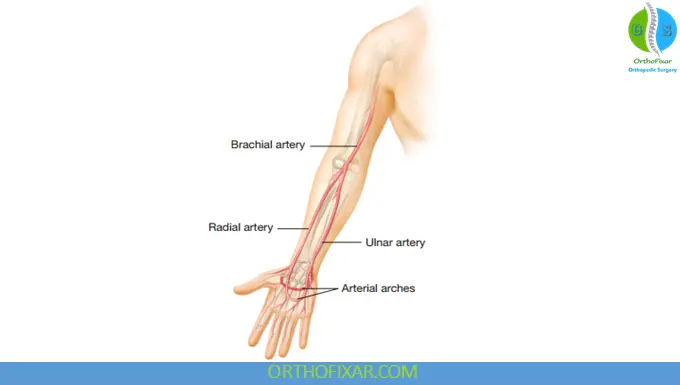
Upper Limb
| Pulse | Anatomical Location | Tip for Palpation |
|---|---|---|
| Brachial Pulse | Medial to the elbow, just distal to the biceps tendon | Use the pads of the index & middle fingers; patient’s arm flexed |
| Radial Pulse | Lateral aspect of the distal forearm, thumb side | Most common peripheral pulse; feel just lateral to the tendon of the flexor pollicis longus |
| Ulnar Pulse | Medial side of the forearm, near the flexor carpi ulnaris | May be obscured by overlying muscle; palpate posterior to the ulna |
Two vascular arches in the hand (deep and superficial palmar arches) interconnect the radial and ulnar arteries, providing collateral flow.
See Also: Radial Pulse Examination
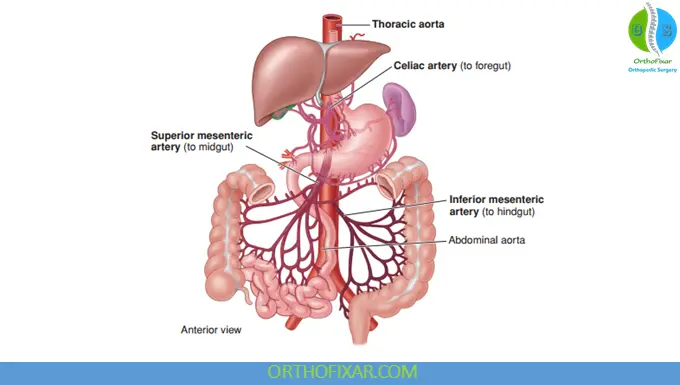
Abdomen
| Pulse | Landmark | Notes |
|---|---|---|
| Aortic (epigastric) | Midline, just above the umbilicus (epigastric region) | Deep, so best felt during deep inspiration |
| Celiac trunk & mesenteric arteries | Not palpable – deep branches; visualized by imaging (CT‑angiography) |
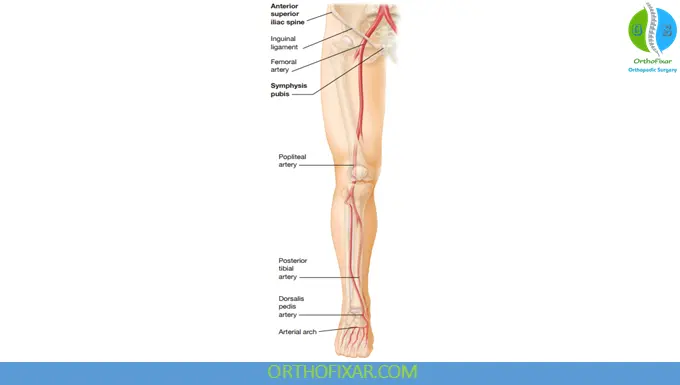
Lower Limb
| Pulse | Anatomical Location | Clinical Relevance |
|---|---|---|
| Femoral | Below inguinal ligament, midway between the ASIS and pubic symphysis | First step in assessing lower‑extremity perfusion |
| Popliteal | Posterior to the knee joint, in the popliteal fossa | Useful for evaluating arterial disease proximal to calf |
| Dorsalis Pedis (DP) | Dorsum of the foot, lateral to the extensor hallucis longus tendon | Indicates distal perfusion; absence may signal occlusion |
| Posterior Tibial (PT) | Posterior to the medial malleolus | Complements DP; both should be assessed in peripheral vascular disease |
Common Arterial Pathologies
Atheroma (Atherosclerotic Plaque) Formation
- Endothelial injury (e.g., oxidative LDL, hypertension) → increased permeability & expression of adhesion molecules.
- Retention of LDL in the intimal proteoglycan matrix → oxidation of LDL (oxLDL).
- Monocyte recruitment → differentiation into macrophages, ingestion of oxLDL → foam cells → formation of fatty streaks (early atheroma).
- SMC migration from media to intima → production of extracellular matrix → development of a fibrous cap over a necrotic lipid‑rich core.
Complex atheroma: Characterized by a thick fibrous cap, abundant inflammatory cells (T‑cells, macrophages), and a necrotic core prone to rupture. Plaque rupture exposes highly thrombogenic material, leading to thrombus formation and potential downstream ischemia.
Thromboembolic Disorders
- Deep Vein Thrombosis (DVT) and Pulmonary Embolism (PE) affect ~1 % of adults >60 y, with a significant fraction presenting as sudden death.
- Upper‑extremity DVT accounts for ~10 % of cases, often iatrogenic (central venous catheters, pacemakers).
- Superficial venous thrombosis can progress to DVT/PE in ~33 % of patients.
Clinical tip: Even though DVT is a venous pathology, arterial wall integrity (e.g., atherosclerotic plaque erosion) can predispose to arterial thromboembolism (e.g., stroke, myocardial infarction). Always evaluate the arterial side in patients with unexplained embolic events.
Collateral Circulation & Anastomoses
When a major artery becomes obstructed, pre‑existing anastomoses between branching networks may undergo arteriogenesis, enlarging to maintain distal perfusion. Clinically, robust collaterals mitigate ischemic symptoms in chronic peripheral arterial disease (PAD).
FAQ
What are the three layers of an artery?
The intima (endothelial lining), media (smooth‑muscle cells with elastic laminae), and adventitia (connective tissue with nerves and vasa vasorum).
How does the internal elastic lamina differ from the external elastic lamina?
The internal elastic lamina separates the intima from the media and is prominent in elastic arteries; the external elastic lamina separates the media from the adventitia, more evident in larger arteries.
Why is the intima considered “metabolically active”?
Endothelial cells synthesize both anti‑ and pro‑thrombotic agents, vasodilators and constrictors, and modulate immune responses—functions essential for vascular homeostasis.
Which arterial segment contributes most to systemic vascular resistance?
Arterioles, because resistance is inversely proportional to the fourth power of the radius (Poiseuille’s law).
What clinical signs suggest a complex atheroma?
Presence of unstable angina, positron‑emission tomography (PET) evidence of inflammation, or high‑resolution MRI showing a thin fibrous cap + large lipid core.
How can one assess endothelial function non‑invasively?
Flow‑mediated dilation (FMD) of the brachial artery, reactive hyperemia index (RHI) via peripheral arterial tonometry, or nitroglycerin‑mediated dilation (NMD) for smooth‑muscle function.
References & More
- Moore KL, et al. Clinically Oriented Anatomy. 8th ed. Philadelphia: Lippincott Williams & Wilkins; 2019.
- Ross R. Atherosclerosis — an inflammatory disease. N Engl J Med. 1999;340(2):115‑126.
- Gimbrone MA, García-Cardeña G. Endothelial cell dysfunction and the pathobiology of atherosclerosis. Circ Res. 2016;118(4):620‑636.
- Mercadante AA, Raja A. Anatomy, Arteries. [Updated 2023 Mar 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: Pubmed
- Tucker WD, Arora Y, Mahajan K. Anatomy, Blood Vessels. [Updated 2023 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: Pubmed


[…] See Also: Arteries Anatomy: Layers, Function & Clinical Insight […]
[…] Artery Disease (PAD), also known as peripheral arterial disease, is a common circulatory condition in […]