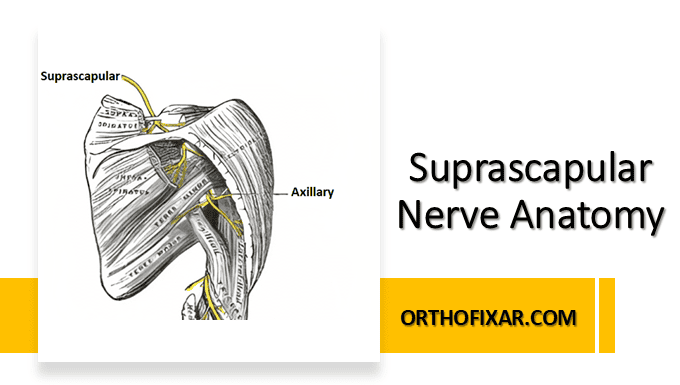
The suprascapular nerve, also known as the nervus suprascapularis, is a mixed motor and sensory nerve that plays a crucial role in shoulder girdle function. This comprehensive guide explores the detailed suprascapular nerve anatomy, including its origin, course, branches, and clinical significance for medical practitioners.
Origin and Formation of the Suprascapular Nerve
Anatomical Origin
The suprascapular nerve anatomy begins at the superior trunk of the brachial plexus, specifically arising from nerve roots C5 and C6. In some anatomical variations, the nerve may receive contributions from C4, making understanding these variations crucial for clinical assessment.
The nerve formation occurs within the posterior triangle of the neck, where the C5 and C6 nerve roots converge to form the superior trunk. From this junction, the suprascapular nerve branches posteriorly, establishing the foundation of suprascapular nerve anatomy.
See Also: Brachial Plexus Anatomy
Nerve Root Contributions
Understanding the nerve root contributions is fundamental to suprascapular nerve anatomy:
- Primary contributors: C5 and C6 nerve roots (95% of cases)
- Variable contributor: C4 nerve root (occasional contribution)
- Rare variations: Isolated C5 or C6 contributions

Detailed Course and Pathway
Cervical and Supraclavicular Regions
The suprascapular nerve anatomy follows a predictable yet complex pathway through multiple anatomical regions. Initially, the nerve travels laterally and posteriorly from the brachial plexus, passing beneath the omohyoid muscle and above the subclavian artery.
In the posterior triangle, the suprascapular nerve anatomy demonstrates its relationship with surrounding structures, including the scalene muscles and cervical fascia. The nerve maintains a relatively superficial position before diving deeper as it approaches the shoulder region.
Passage Through the Suprascapular Notch
One of the most clinically significant aspects of suprascapular nerve anatomy involves its passage through the suprascapular notch. The nerve passes beneath the superior transverse scapular ligament (also called the suprascapular ligament), while the suprascapular artery typically passes above this ligament.
This anatomical relationship creates a potential compression site, making the suprascapular notch a critical landmark in suprascapular nerve anatomy. The dimensions and shape of the suprascapular notch vary significantly among individuals, influencing the risk of nerve entrapment.
Intrascapular Course
After passing through the suprascapular notch, the suprascapular nerve anatomy continues within the supraspinous fossa. The nerve travels laterally along the base of the scapular spine, maintaining intimate contact with the supraspinatus muscle.
The nerve then curves around the lateral border of the scapular spine, passing through the spinoglenoid notch (also called the great scapular notch) to enter the infraspinous fossa. This transition represents another critical point in suprascapular nerve anatomy where compression can occur.
Muscular Innervation Pattern
Supraspinatus Muscle Innervation
The suprascapular nerve anatomy includes direct motor innervation to the supraspinatus muscle. This innervation occurs early in the nerve’s course, with motor branches arising before the nerve passes around the scapular spine.
The supraspinatus receives multiple motor branches, ensuring robust innervation for this crucial rotator cuff muscle. Understanding this aspect of suprascapular nerve anatomy is essential for predicting functional deficits in nerve injuries.
Infraspinatus Muscle Innervation
After rounding the scapular spine, the suprascapular nerve anatomy continues with innervation of the infraspinatus muscle. The infraspinatus receives motor branches throughout the nerve’s course in the infraspinous fossa, providing comprehensive neural control.
The innervation pattern demonstrates the functional importance of intact suprascapular nerve anatomy for external rotation and shoulder stability. Damage to the nerve at different levels produces varying patterns of muscle weakness.
Sensory Distribution and Functions
Articular Branches
The sensory component of suprascapular nerve anatomy includes articular branches that innervate the glenohumeral joint, acromioclavicular joint, and associated capsular structures. These sensory fibers contribute significantly to proprioception and pain sensation in the shoulder region.
Understanding the sensory distribution helps explain the pain patterns observed in the nerve pathology. The articular innervation makes the nerve clinically relevant beyond its motor functions.
Cutaneous Contributions
While primarily motor, suprascapular nerve anatomy includes minimal cutaneous sensory contributions. These are typically limited to small areas over the shoulder region and may vary significantly among individuals.
Anatomical Variations and Clinical Implications
Common Anatomical Variations
Suprascapular nerve anatomy demonstrates several clinically relevant variations:
Branching Patterns: The nerve may show variations in its branching pattern to the supraspinatus and infraspinatus muscles. Some individuals have separate nerve branches for each muscle, while others show a common trunk with later division.
Passage Variations: The relationship with the suprascapular ligament may vary, with some nerves passing through ossified ligaments or through separate foramina in the scapula.
Size and Caliber: The diameter and fascicular organization of the nerve show individual variations that may influence susceptibility to compression injuries.
Fascial Relationships and Anatomical Boundaries
Fascial Planes
The suprascapular nerve anatomy involves passage through multiple fascial planes. The nerve initially travels within the cervical fascia before entering the supraspinous and infraspinous fascial compartments.
These fascial relationships create potential spaces where pathology can develop, including nerve entrapment, cyst formation, and inflammatory conditions affecting nerve function.
Anatomical Landmarks
Key anatomical landmarks in suprascapular nerve anatomy include:
- Suprascapular notch: Primary compression site
- Scapular spine: Landmark for nerve localization
- Spinoglenoid notch: Secondary compression site
- Coracoid process: Surgical landmark for nerve approach
Clinical Pathology and Dysfunction
Suprascapular Nerve Entrapment
Understanding suprascapular nerve anatomy is essential for recognizing entrapment syndromes. The most common sites of compression occur at:
- Suprascapular notch: Most frequent site of entrapment
- Spinoglenoid notch: Secondary compression location
- Fascial planes: Less common but clinically significant

Traumatic Injuries
The anatomical course makes the suprascapular nerve vulnerable to various traumatic injuries. Traction injuries commonly occur during shoulder dislocations or high-energy trauma affecting the brachial plexus region.
Direct trauma to the scapular region can also damage the nerve, particularly in its more superficial course through the supraspinous and infraspinous fossae.
Diagnostic Considerations
Electrodiagnostic Testing
Nerve conduction studies and electromyography require understanding of the nerve’s course and innervation pattern for accurate interpretation.
The anatomical relationships help localize lesions and determine the extent of nerve involvement, crucial for treatment planning and prognosis.
Imaging Correlations
Modern imaging techniques, including MRI and ultrasound, rely on detailed knowledge of suprascapular nerve anatomy for accurate interpretation. The nerve’s relationship to surrounding structures enables identification of pathological changes and compression sites.
Surgical Anatomy and Clinical Applications
Surgical Approaches
Multiple surgical approaches to the suprascapular nerve require thorough understanding of its anatomy:
Posterior approach: Direct access through the infraspinous fossa Superior approach: Access through the suprascapular notch region Arthroscopic techniques: Minimally invasive approaches guided by anatomical landmarks
Nerve Decompression Procedures
Surgical decompression of the suprascapular nerve involves release at specific anatomical sites. Understanding the precise anatomy ensures complete decompression while avoiding injury to surrounding structures.
The relationship between the nerve and the superior transverse scapular ligament is particularly important for successful decompression at the suprascapular notch.
References & More
- Basta M, Sanganeria T, Varacallo MA. Anatomy, Shoulder and Upper Limb, Suprascapular Nerve. [Updated 2022 Oct 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557880/
- Kostretzis L, Theodoroudis I, Boutsiadis A, Papadakis N, Papadopoulos P. Suprascapular Nerve Pathology: A Review of the Literature. Open Orthop J. 2017;11:140-153. [PMC free article] [PubMed]
- Shin C, Lee SE, Yu KH, Chae HK, Lee KS. Spinal root origins and innervations of the suprascapular nerve. Surg Radiol Anat. 2010 Mar;32(3):235-8. [PubMed]
- Avery BW, Pilon FM, Barclay JK. Anterior coracoscapular ligament and suprascapular nerve entrapment. Clin Anat. 2002 Nov;15(6):383-6. [PubMed]